Translate this page into:
Tetany in a Patient with Gastroesophageal Reflux Disease
Corresponding author: Subrahmanian Sathiavageesan, Department of Nephrology, Sundaram Hospital, Trichy, Tamil Nadu, India. E-mail: spssubrahmanian@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Sathiavageesan S. Tetany in a Patient with Gastroesophageal Reflux Disease. Indian J Nephrol. 2024;34:676-7. doi: 10.25259/IJN_239_2024
Dear Editor,
Proton pump inhibitors (PPI) are widely prescribed drugs and generally well tolerated. However, prolonged intake of PPI increases risk of micronutrient deficiency (iron, magnesium, and vitamin B12), infections, and kidney disease.1 We report the occurrence of tetany due to hypomagnesemia in a patient who had been on long-term PPI therapy for gastroesophageal reflux.
Our patient was a 32-year-old man, who had been receiving pantoprazole 40 mg/day and domperidone 20 mg/day for 5 years for refractory gastroesophageal reflux disease. Attempts to stop pantoprazole resulted in resurgence of reflux symptoms. He presented during peak summer with recurrent muscle cramps to different hospitals where heat cramp was diagnosed and treated symptomatically. There was no respite of symptoms and he presented to our emergency room with generalized muscle cramps. He had excess fatigue and cramping was aggravated by ambulation. There was no associated fever, vomiting, or diarrhea. He consumed alcohol occasionally and denied intake of illicit drugs. He did not have diabetes mellitus or hypertension, and he was not taking any other medications. Family history was unremarkable.
On arrival, he was conscious, oriented, afebrile lean-built, and his vital signs were normal. Inflation of blood pressure cuff provoked tetany [Figure 1a]. Plantar reflex was flexor, muscle power and sensory system examination werenormal and deep tendon reflexes were brisk. A diagnosis of tetany was made.
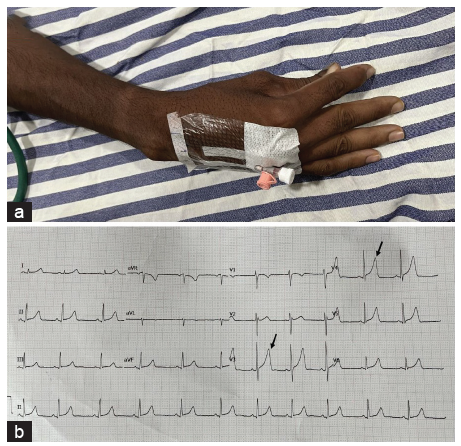
- (a) Tetany induced by inflating blood pressure cuff. (b) Electrocardiogram reveals tall, peaked T-waves in precordial leads (black arrows) when serum potassium was 3.0 mmol/L and serum magnesium was 0.9 mg/dl (reference: 1.6–2.5 mg/dl).
Complete blood count; blood sugar; and serum levels of creatinine, sodium, and total protein and albumin were normal. He had hypokalemia (K 3.0 mmo/L) and hypocalcemia (calciumtotal 7.9 mg/dl; calciumionized 4.1 mg/dl). Serum phosphorous was normal, and intact parathormone was suppressed (3.1 pg/mL). Arterial blood gas analysis revealed normal pH and bicarbonate. Electrocardiogram revealed tall, peaked T-waves [Figure 1b]. Tall T-waves, despite hypokalemia arouse suspicion of hypomagnesemia. Serum magnesium was low (0.9 mg/dl). Urinary fractional excretion of magnesium (FEMg) was 1.3%, implying renal conservation of magnesium and loss through extra-renal route (gastrointestinal tract). A diagnosis of PPI-induced hypomagnesemia with resultant hypocalcemia and hypokalemia was made.
He received intravenous followed by oral magnesium replacement along with intravenous calcium gluconate and oral potassium chloride supplementation. Pantoprazole was stopped. Serum magnesium, calcium, and potassium returned to normal by the third day. Tetany resolved and T-wave amplitude normalized.
Hypomagnesemic tetany due to PPI was reported as early as 20062 and further studies have established the association.3,4 An estimated 2–36% of patients on PPI develop hypomagnesemia.4 PPI impairs the gastrointestinal absorption of magnesium by inhibiting Transient Receptor Potential Channel Melastatin 6 and 7 (TRPM6/7) responsible for magnesium absorption in the gut.5 Prolonged use (>1 year), old age, and concomitant diuretic therapy are predisposing factors for hypomagnesemia.
Fractional excretion of magnesium (FEMg) is a useful test to differentiate renal from gastrointestinal loss of magnesium. FEMg of 3% or above implies renal magnesium wasting while a lesser value indicates renal magnesium conservation in the face of gastrointestinal magnesium loss.6 Hypomagnesemia induces hypoparathyroidism by reducing parathormone secretion and promoting end organ resistance to parathormone.6 While hypoparathyroidism contributes to hypocalcemia, hypokalemia in hypomagnesemia is the result of renal potassium wasting. Tall T-waves despite hypokalemia should arouse suspicion of hypomagnesemia.6
Conflicts of interest
There are no conflicts of interest.
References
- Perils and pitfalls of long-term effects of proton pump inhibitors. Expert Rev Clin Pharmacol. 2013;6:443-51.
- [CrossRef] [PubMed] [Google Scholar]
- Proton-pump inhibitors and hypomagnesemic hypoparathyroidism. N Engl J Med. 2006;355:1834-6.
- [CrossRef] [PubMed] [Google Scholar]
- Hypomagnesaemia due to proton-pump inhibitor therapy: A clinical case series. QJM. 2010;103:387-95.
- [CrossRef] [PubMed] [Google Scholar]
- Proton pump inhibitors and hypomagnesemia: A meta-analysis of observational studies. Medicine (Baltimore). 2019;98:e17788.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mechanisms of proton pump inhibitor-induced hypomagnesemia. Acta Physiol (Oxf). 2022;235:e13846.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







