Translate this page into:
The Utility of the Creatinine Excretion to Production Ratio and the Plasma Creatinine and Cystatin C Based Kinetic Estimates of Glomerular Filtration Rates in Critically Ill Patients with Sepsis
Address for correspondence: Prof. Azrina Md Ralib, Department of Anaesthesiology and Intensive Care, International Islamic University Malaysia, Bandar Indera Mahkota, 25200 Kuantan, Pahang, Malaysia. E-mail: azrinar@iium.edu.my
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Creatinine kinetics denotes that under steady-state conditions, creatinine production (G) will equal creatinine excretion rate (E). The glomerular filtration (GFR) is impaired when excretion is less than production. The kinetic estimate of GFR (keGFR) and E/G ratio were proposed as a more accurate estimate of GFR in acute settings with rapidly changing kidney function. We evaluated keGFR and E/G to diagnose AKI, predict recovery, death or dialysis.
Methods:
This is a prospective observational study of critically ill patients. Inclusion criteria were patients >18 years old with sepsis, defined as clinical infection with an increase in SOFA score >2, and plasma procalcitonin >0.5 ng/mL. Plasma creatinine and Cystatin C were measured on ICU admission and 4 h later, and their keGFR was calculated. Urine creatinine and urine output were measured over 4 h to calculate the E/G ratio.
Results:
A total of 70 patients were recruited, of which 49 (70%) had AKI. Of these, 33 recovered within 3 days, and 15 had a composite outcome of death or dialysis. Day 1 keGFRCr and keGFRCysC discriminated AKI from non-AKI with AUCs of 0.85 (95% Confidence interval: 0.74–0.96), and 0.86 (0.76–0.97), respectively. The E/G ratio predicted AKI recovery (AUC: 0.81 (0.69–0.97)). The keGFRs were not predictive of death or dialysis, whereas E/G was predictive (AUC: 0.76 (0.63–0.89).
Conclusion:
keGFR was strongly diagnostic of AKI. The E/G ratio predicted AKI recovery and a composite outcome of death and dialysis.
Keywords
Creatinine
critical illness
Cystatin C
glomerular filtration rate
sepsis
Introduction
Acute kidney injury (AKI) is an independent risk factor that contributes to morbidity and mortality in critically ill patients. In a Malaysian population, AKI occurred in 65% of patients, mainly attributed to sepsis, higher compared to studies in other countries.[12] Current diagnosis of AKI is based on the surrogates of filtration function, namely creatinine and urine output.[3] It is recognized that injury biomarkers measured in the urine or plasma may provide earlier indications of AKI than plasma creatinine. However, few have reached clinical utility, and their use is complicated by the heterogeneity of the ICU population. Furthermore, they are only available at a high cost.
Kinetic estimate of GFR (keGFR) was proposed by Chen[4] to be a more accurate estimate of GFR in acute settings, where kidney function can change rapidly in the critically ill. It considers the changes in plasma (or serum) creatinine over time, creatinine production rate, and the volume of distribution. keGFR has been shown to be a better predictor of AKI and AKI recovery compared to the eGFRs.[56] Since then, many studies have shown the utility of keGFR in diagnosing AKI, staging severity, predicting renal recovery, medication dosing, and in cardiac surgical patients.[7–10]
In a steady state (unchanging GFR), the creatinine production rate (G) must equal the creatinine excretion rate (E). If production exceeds excretion, glomerular filtration function (GFR) is impaired.[11] On the contrary, if excretion exceeds production, it may indicate a recovering GFR following a reduction in GFR. Creatinine production cannot be measured directly, but like the estimating equations for GFR, there are estimating equations for production. The E/G ratio provides additional information on the state of GFR. Utilizing either the E/G ratio or keGFR may offer a cheap way to evaluate the kidney function in critically ill patients. We investigated the ability of the keGFR and E/G to diagnose AKI, predict its recovery, and predict the hard outcome of death or dialysis in the ICU. In addition, we explored the association of AKI severity stages with keGFR severity classifications.
Methods
This was a prospective observational study at Hospital Tengku Ampuan Afzan, Kuantan and Sultan Ahmad Shah Medical Center (SASMEC@IIUM). The study was registered under the Malaysian National Medical Research Register (NMRR-14-1897-21447). Ethical approval was obtained from the Malaysian Medical Ethics and Research Committee (MREC number: P15-1597) and the International Islamic University Ethics Committee (IREC number: 511). Consent from legally accepted patient representatives was obtained. All patients admitted to the ICU during the study period were screened for inclusion. The inclusion criteria were patients older than 18 years, ICU stay longer than 48 h with sepsis, and plasma procalcitonin (PCT) > 0.5 ng/mL. Sepsis was defined as clinical infection and acute increase in SOFA score of more than two organs.[12] The exclusion criteria were patients who already had severe AKI on admission, defined as needing dialysis, creatinine three times the baseline, or urine output of less than 0.3 mL/kg/h.
Plasma and urinary samples were collected on admission and at 4 and 8 h on thefirst day, then two samples daily 4 h apart for thefirst 3 days of ICU admission. Urine samples were centrifuged at 2000 rpm for 5 min, and the supernatant was stored at –80°C. Blood samples were centrifuged at 3600 rpm for 15 min, and the plasma was stored at –80°C. PCT was assayed using the rapid PCT quantitative test (Wondfo Biotech). Plasma and urine creatinine were assayed using Olympus AU2700™ chemistry-immunoanalyzer (Olympus, Philadelphia, USA), and 4-h creatinine clearance was calculated.[13] Baseline creatinine could not be obtained from clinical records; therefore, it was estimated using back-calculation of the Modified Diet in Renal Disease (MDRD) equation based on an estimated glomerular filtration rate (eGFR) of 75 mL/min.[1415] AKI was defined as a plasma creatinine increase of greater than 26.4 umol/L or 50% of baseline within 24 h of ICU admission or urine output of less than 0.5 mL/kg/h for the past 6 h. AKI recovery (AKIrec) was defined as the return of plasma creatinine to less than 1.5 times the baseline value or less than 30 μmol/L (0.35 mg/dL), or reversal of oliguria within 3 days of ICU admission.[16] Estimated GFR (eGFR) values were calculated using the Cockcroft–Gault,[17] MDRD,[18] and CKD-EPI formulas.[18] keGFR was calculated using the formula by Chen.[46] The excretion rate (E) was calculated using the urinary volume measured over 4 h and the urinary creatinine concentration measured from this 4-h volume.
Statistical analysis
Results are presented as mean ± SD for normally distributed variables or median (inter-quartile range) for non-normally distributed variables. Comparison of variables between the two groups was analyzed using the independent t test for normally distributed variables or the Mann–Whitney test for non-normally distributed variables. Differences between the three groups were analyzed using one-way analysis of variance (ANOVA) with post-hoc least significant difference analysis. Categorical variables were compared with Chi-square test. The diagnostic and predictive performances were assessed by the area under the curve (AUC) of the receiver operating characteristic (ROC) curve of the sensitivity verse 1-specificity. The ideal cutoff point was defined as the measured quantity, which maximized sensitivity and specificity.
Results
Demographic and clinical characteristics
A total of 70 patients were recruited, of which 49 (70%) had AKI. Of these, 36 (51.4%) had AKI based on creatinine criteria alone, and 38 (54.3%) had AKI based on urine output criteria alone. Out of 49 patients with AKI, 33 (67.3%) recovered within 3 days. The remaining 16 (32.7%) had persistent AKI. Patients' flow is shown in Figure 1. Table 1 shows the demographic and clinical characteristics and outcomes of recruited patients. Of the 70 patients, 12 (17.1%) died within 30 days of ICU admission and eight (11.4%) needed dialysis. Fifteen patients (21.4%) had the composite outcome of death or dialysis.

- Patient flow
| Variables | All patients (n=70) |
|---|---|
| Age (years) | 51.0±17.6 |
| Gender (male) | 42 (60.0) |
| Weight (kg) | 66±17 |
| Height (cm) | 162±8 |
| Baseline SOFA Score | 5.6±3.2 |
| Baseline APACHE II Score | 14.3±5.6 |
| Category | |
| Medical | 51 (72.9) |
| Surgical | 19 (27.1) |
| Primary admission diagnoses | |
| Cardiovascular | 6 (8.6) |
| Gastrointestinal/Hepatobiliary/Pancreas | 13 (18.6) |
| Infective | 7 (10.0) |
| Renal Neurological | 2 (2.9) |
| Respiratory | 2 (2.9) |
| Trauma | 26 (37.1) |
| Connective tissue/autoimmune | 3 (4.3) |
| Endocrine | 4 (5.7) |
| Hematology | 1 (1.4) |
| Dialysis | 8 (11.4) |
| Death at 30 days | 12 (17.1) |
| Dialysis or Death at 30 days | 15 (21.4) |
| Mechanical Ventilation (MV) | 56 (80.0) |
| Length of MV (days) (n=46) | 2.7 (1.6-6.8) |
| Length of ICU stay (days) (n=58) | 4.4 (2.8-7.9) |
| Length of hospital stay (days) (n=58) | 13.9 (8.7-24.6) |
Data expressed as mean±SD, n (%), or median (lower quartile - upper quartile). APACHE II Score: Acute Physiological and Chronic Health Evaluation II Score. SOFA Score: Sequential Organ Failure Assessment
Profile of plasma Creatinine, plasma CysC, their GFR derivatives, and E/G ratio
Figure 2 shows the line graph between patients with AKI and no AKI for plasma biomarkers and their eGFR equations. Plasma creatinine and Cystatin C were higher in patients with AKI versus no AKI. Correspondingly, their GFR derivatives were lower in patients with AKI compared to no AKI.
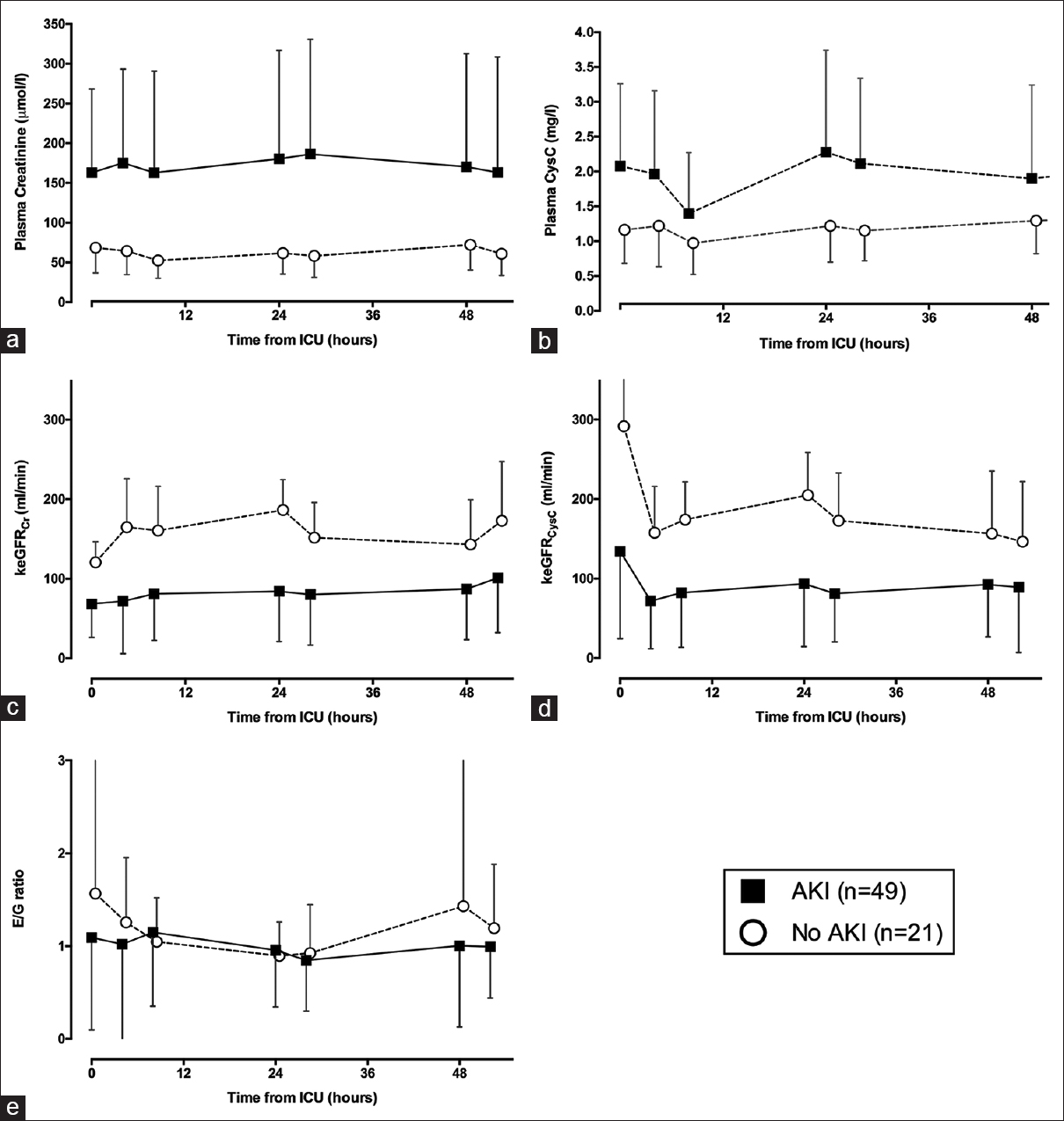
- Line graph between AKI and No AKI for (a) Plasma Creatinine, (b) Plasma Cystatin C, (c) keGFRCr, (d) keGFRCysC, and (e) E/G ratio. Each point is the mean for all patients at that time. The 95% confidence interval is shown for each data point. For clarity's sake, we display only one side of the CI
Diagnosis of AKI
Plasma creatinine and CysC were diagnostic of AKI throughout the 3 days of ICU admission [Figure 3]. Similarly, keGFRCr and keGFRCysC were diagnostic of AKI throughout the 3 days, whereas the E/G ratio was not diagnostic. Day 1 keGFRCr and keGFRCysC performed best in the diagnosis of AKI, with an AUC of 0.85 (0.74–0.96) and 0.86 (0.76–0.97), and an ideal cutoff point of 103 and 100 mL/min, respectively [Table 2]. Day 1 E/G ratio was also diagnostic of AKI, but with a lower AUC of 0.69 (0.56–0.82).
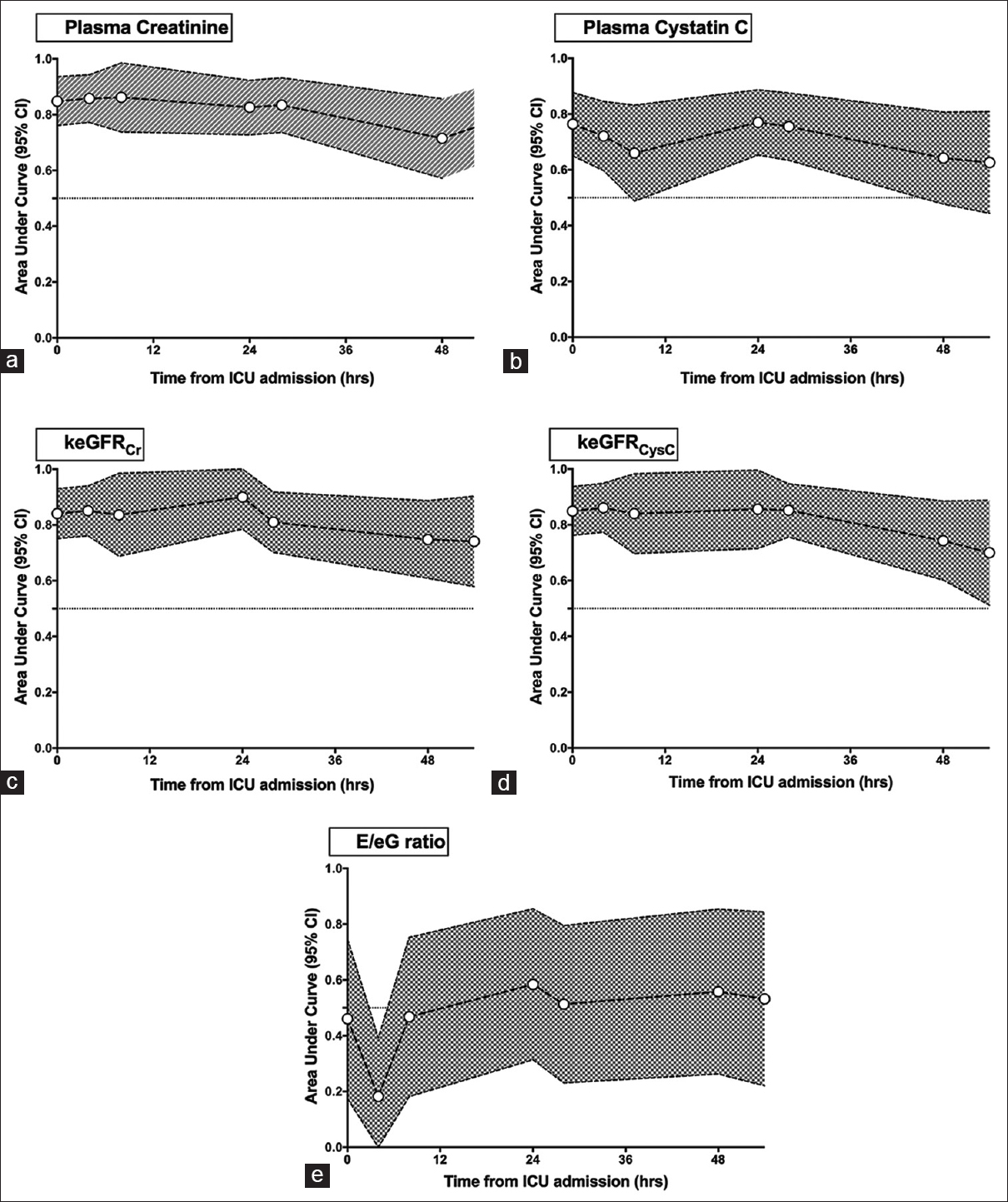
- Time-dependent performance for the diagnosis of AKI (a) Plasma Creatinine, (b) Plasma Cystatin C, (c) keGFRCr, (d) keGFRCysC, and (e) E/G ratio. The shaded area represents the 95% Confidence interval. keGFR: kinetic estimate of glomerular filtration rate, E/G ratio: production/excretion ratio of creatinine
| Variables | AUC (95% CI) | Ideal Cutoff Point | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) |
|---|---|---|---|---|---|---|
| Diagnosis of AKI (n=49) | ||||||
| pCreatinine | 0.85 (0.76-0.94) | 95 mmol/L | 0.73 (0.60-0.85) | 0.86 (0.71-1) | 0.92 (0.84-1) | 0.58 (0.41-0.75) |
| pCysC | 0.76 (0.64-0.87) | 1.5 mg/L | 0.62 (0.49-0.76) | 0.86 (0.71-1) | 0.91 (0.81-1) | 0.50 (0.34-0.66) |
| keGFRCr | 0.85 (0.74-0.96) | 103 mL/min | 0.86 (0.71-1) | 0.75 (0.62-0.88) | 0.62 (0.44-0.80) | 0.92 (0.83-1) |
| keGFRCysC | 0.86 (0.76-0.97) | 100 mL/min | 0.86 (0.71-1) | 0.80 (0.68-0.91) | 0.67 (0.49-0.84) | 0.92 (0.84-1) |
| E/eG ratio | 0.60 (0.45-0.75) | 0.66 | 0.86 (0.71-1) | 0.42 (0.28-0.56) | 0.39 (0.25-0.53) | 0.87 (0.73-1) |
| Prediction of AKI recovery (n=33) in patients with AKI (n=49) | ||||||
| pCreatinine | 0.79 (0.65-0.94) | 175 mmol/L | 0.69 (0.46 to0.91) | 0.82 (0.69-0.95) | 0.65 (0.42-0.87) | 0.84 (0.72-0.97) |
| pCysC | 0.70 (0.53-0.86) | 1.53 mg/L | 0.81 (0.62-1) | 0.55 (0.38-0.72) | 0.46 (0.28-0.65) | 0.86 (0.71-1) |
| keGFRCr | 0.74 (0.59-0.88) | 55 mL/min | 0.63 (0.46-0.81) | 0.93 (0.81-1.1) | 0.95 (0.85-1) | 0.56 (0.37-0.75) |
| keGFRCysC | 0.79 (0.65-0.92) | 47 mL/min | 0.76 (0.60-0.91) | 0.81 (0.62-1) | 0.88 (0.75-1) | 0.65 (0.44-0.86) |
| E/G ratio | 0.81 (0.69-0.94) | 0.59 | 0.81 (0.70-0.91) | 0.83 (0.62-1) | 0.96 (0.9-1) | 0.48 (0.26-0.69) |
| Prediction of death or dialysis (n=15) | ||||||
| pCreatinine | 0.65 (0.48-0.81) | 163 mmol/L | 0.6 (0.35-0.85) | 0.78 (0.67-0.89) | 0.43 (0.22-0.64) | 0.88 (0.78-0.97) |
| pCysC | 0.58 (0.42-0.73) | 1.51 mg/dL | 0.6 (0.35-0.85) | 0.57 (0.44-0.71) | 0.28 (0.13-0.44) | 0.84 (0.72-0.96) |
| keGFRCr | 0.61 (0.43-0.78) | 55 mL/min | 0.69 (0.56-0.81) | 0.64 (0.39-0.89) | 0.88 (0.77-0.98) | 0.36 (0.17-0.55) |
| keGFRCysC | 0.64 (0.45-0.83) | 55 mL/min | 0.69 (0.56-0.81) | 0.64 (0.39-0.89) | 0.88 (0.77-0.98) | 0.36 (0.17-0.55) |
| E/G ratio | 0.76 (0.63-0.89) | 0.68 | 0.76 (0.65-0.87) | 0.73 (0.51-0.96) | 0.91 (0.83-0.99) | 0.46 (0.26-0.66) |
keGFR: kinetic estimate of glomerular filtration rate, E/G ratio: production/excretion ratio of creatinine
Prediction of AKI recovery
In 49 patients with AKI, 33 (67.3%) recovered within 3 days. In these cases, the E/G ratio was strongly predictive of AKI recovery with the highest AUC of 0.81 (0.69–0.94) [Table 2]. The ideal cutoff point of the E/G ratio in the prediction of AKI recovery was 0.59 (representing that the excretion rate is 59% of the production rate). keGFR derivatives for creatinine and plasma CysC were also predictive, with lower AUCs.
Prediction of death or dialysis
Twelve patients (17.1%) died, eight (11.4%) needed dialysis, and 15 (21.4%) either died or needed dialysis. Plasma creatinine, CysC, and their eGFR derivatives were not predictive of death or dialysis. On the contrary, the E/G ratio was predictive, with an AUC of 0.76 (0.63–0.89) and an ideal cutoff point of 0.68.
Discussion
Seventy percent of the recruited patients had AKI based on either plasma creatinine or urine output criteria. Of these, more than half recovered within 3 days of admission. Plasma creatinine, CysC, and their keGFR measured on ICU admission were diagnostic of AKI; in contrast, the E/G ratio was not. E/G ratio was useful for the prediction of recovery in patients with AKI and in the prediction of death or dialysis.
A high proportion (70%) of our patients had AKI. This may be due to the strict inclusion criteria of our study. Apart from using the Sepsis-3 definition, we also included PCT of greater than 0.5 ng/mL, which further specified our target population as having a bacterial infection. Many of these patients were of a high severity stage due to the presence of already two organ failures; thus, the resultant incidence of AKI was also higher compared to general ICU populations. We showed that both keGFRCr and keGFRCysC were strongly diagnostic of AKI with an AUC of greater than 0.8. This is consistent with other studies. A study of 56 kidney transplant patients showed that keGFR was predictive of delayed graft function, whereas creatinine was not.[6] In a large study involving 4000 cardiac surgery patients, keGFR in the presence of unchanged creatinine level predicted AKI and mortality.[19] On the contrary, we showed here that keGFR had similar AUCs to that of plasma creatinine.
keGFR calculations consider the changes of creatinine over time, creatinine production rate, and the volume of distribution. Thus, in rapidly changing kidney functions as in critically ill patients, this estimate is suggested to be more useful.[4] The limitations of keGFR include its complex mathematical calculations. In addition, reductions in creatinine production associated with muscle mass loss and changes in the volume of distribution in critically ill patients may be an important confounder for its utility for a long-term outcome.[20]
About 60% of our AKI patients recovered within 3 days of ICU admission, similar to another study which showed that about 51% of their ICU patients had short-term recovery defined as resolution of plasma creatinine and oliguria within 48 h.[16] In contrast to the diagnosis of AKI, we showed that keGFR performed inferior in the prediction of AKI recovery in our cohort, with a lower AUC of 0.74 and 0.79 for creatinine and CysC, respectively, with almost similar AUCs to their plasma concentrations. A study by Dewitte et al.[16] showed that keGFR provided the best AUC for renal recovery with an AUC of 0.87 compared to other plasma biomarkers, that is, NGAL, TIMP-2, and IGFBP7.
Of all the derivatives, we showed that the E/G ratio performed the best for AKI recovery. In a proof-of-concept paper, Endre et al.[5] retrospectively analyzed the utility of the E/G ratio in 482 critically ill patients. The E/G ratio predicted AKI and its recovery defined by changes in creatinine 12 h later. The ratio was predictive in a subgroup of 66 chronic kidney disease patients. In a study of 56 renal transplant patients, both E/G and keGFR improved risk prediction for delayed graft function.[6] In this study, we showed that the E/G ratio was strongly predictive of AKI recovery with an AUC of greater than 0.8. Under steady state, creatinine production equals to creatinine excretion rate.[11] E/G ratio provides additional information on the current state of the patients' GFR in relation to the steady state. An E/G ratio of less than 1 (production exceeds excretion) indicates that the patient's GFR is falling from the steady state, whereas a ratio of more than 1 (excretion exceeds production) indicates that the patient's GFR is recovering from a prior fall. In predicting the occurrence of death or dialysis, we showed that the E/G ratio had the highest predictive performance, whereas keGFR of both creatinine and CysC were not predictive. To the best of our knowledge, this is thefirst study that demonstrates this.
Limitations of the study
The study has several limitations,First, we only recruited sepsis patients with PCT greater than 0.5 ng/mL; this may limit the generalizability of the finding to the general ICU population. Second, we estimated the baseline creatinine as we did not have data on measured baseline creatinine; this may over/underestimate the number of AKI in our setting. Third, baseline creatinine could not be obtained from clinical records; therefore, it was estimated using back-calculation of the MDRD equation based on eGFR of 75 mL/min.[1415] This has been shown to be a poor method.[15]
Conclusion
AKI occurred is common in critically ill patients with sepsis. keGFR of both creatinine and CysC was useful for the diagnosis of AKI. E/G ratio was useful for the prediction of recovery in patients with AKI, and prediction of death or dialysis.
Financial support and sponsorship
This study was funded by the Ministry of Higher Education Fundamental Research Grant Scheme (FRGS/1/2019/SKK02/UIAM/02/1, FRGS19-184-0793).
Conflicts of interest
There are no conflicts of interest.
References
- Acute kidney injury in Malaysian intensive care setting: Incidences, risk factors, and outcome. Indian J Crit Care Med. 2018;22:831-5.
- [Google Scholar]
- Acute kidney injury in a Malaysian intensive care unit: Assessment of incidence, risk factors, and outcome. J Crit Care. 2015;30:636-42.
- [Google Scholar]
- KDIGO clinical practice guidelines for acute kidney injury? Nephron Clin Pract. 2012;120:c179-83. doi: 10.1159/000339789
- [Google Scholar]
- Retooling the creatinine clearance equation to estimate kinetic GFR when the plasma creatinine is changing acutely. J Am Soc Nephrol. 2013;24:877-88.
- [Google Scholar]
- Timely diagnosis of acute kidney injury using kinetic eGFR and the creatinine excretion to production ratio, E/eG-Creatinine can be useful! Nephron. . 2016;132:312-6.
- [Google Scholar]
- Kinetic estimation of GFR improves prediction of dialysis and recovery after kidney transplantation? PLoS One. 2015;10:e0125669. doi: 10.1371/journal.pone. 0125669
- [Google Scholar]
- A bedside clinical tool using creatinine kinetics to predict worsening renal injury and early recovery. Clin Kidney J. 2019;12:248-52.
- [Google Scholar]
- The clinical utility of kinetic glomerular filtration rate. Clin Kidney J. 2017;10:202-8.
- [Google Scholar]
- The value of kinetic glomerular filtration rate estimation on medication dosing in acute kidney injury. PLoS One. 2019;14:e0225601.
- [Google Scholar]
- Estimated GFR and AKI outcome prediction model for post cardiac surgery patients. Anesth Analg. 2014;118:S94.
- [Google Scholar]
- A simple method to detect recovery of glomerular filtration rate following acute kidney injury. BioMed Res Int. 2014;2014:542069.
- [Google Scholar]
- The third international consensus definitions for sepsis and septic shock (sepsis-3) JAMA. 2016;315:801-10.
- [Google Scholar]
- Four hour creatinine clearance is better than plasma creatinine for monitoring renal function in critically ill patients. Crit Care. 2012;16:R107.
- [Google Scholar]
- A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Ann Intern Med. 1999;130:461.
- [Google Scholar]
- Back-calculating baseline creatinine with MDRD misclassifies acute kidney injury in the intensive care unit. Clin J Am Soc Nephrol. 2010;5:1165-73.
- [Google Scholar]
- Kinetic eGFR and novel AKI biomarkers to predict renal recovery. Clin J Am Soc Nephrol. 2015;10:1900-10.
- [Google Scholar]
- A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604-12.
- [Google Scholar]
- Kinetic estimated glomerular filtration rate and acute kidney injury in cardiac surgery patients. J Crit Care. 2016;31:249-54.
- [Google Scholar]
- Reduced production of creatinine limits its use as marker of kidney injury in sepsis. J Am Soc Nephrol. 2009;20:1217-21.
- [Google Scholar]







