Translate this page into:
Unilateral xanthogranulomatous pyelouretritis with a functioning kidney
Address for correspondence: Dr. B. Sureka, Department of Radiodiagnosis, VMMC and Safdarjung Hospital, Resident Doctors Hostel, Room 57, New Delhi 110 029, India. E-mail: binitsureka@hotmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 36-year-old male presented to the emergency department with left flank pain, intermittent hematuria and dysuria for 20 days. On examination, he was drowsy and afebrile, with a pulse rate of 76/min, blood pressure of 140/80 mmHg and respiratory rate of 16/min. Laboratory investigations revealed raised erythrocyte sedimentation rate (ESR) and normal renal function. Urinalysis showed microscopic hematuria with few pus cells.
Ultrasonography revealed normal-sized kidneys with moderate hydronephrosis of the left kidney. Renal pelvis showed a large calculus measuring 2.5 cm (2 cm. Homogenous echogenic areas were seen in the renal pelvis and proximal periureteric region [Figure 1]. Right kidney and urinary bladder were normal. Contrast-enhanced computed tomography showed normal-sized and normally functioning kidneys. Calculus was seen in the left renal pelvis with moderate hydronephrosis. The renal pelvis) and proximal ureter showed thickening and enhancement of its wall with surrounding thick rim of fat-attenuating component (−85 to − 100 HU) [Figure 2]. A magnetic resonance imaging showed circumferential layers of varying signal intensity on axial scans and calculus as a signal void in the center. The intermediate granulation tissue showed enhancement in the left renal pelvis and periureteric region. The peripheral hyperintense rim on T1 was suppressed on the fat sat sequence, confirming its lipid nature [Figure 3]. Based on these imaging findings, a diagnosis of xanthogranulomatous etiology was considered.
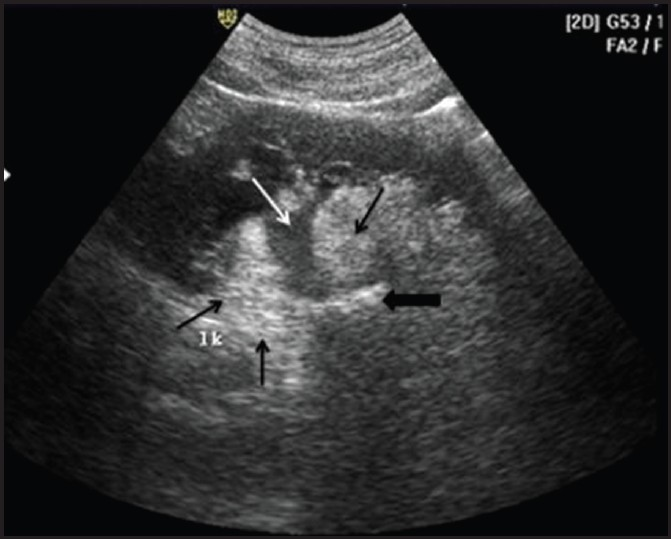
- Longitudinal ultrasound scan of left kidney showing moderate hydronephrosis (white arrow) with echogenic areas (black arrows) surrounding the renal pelvis and proximal ureter. A calculus (black arrowhead) of 2.5 cm × 2.3 cm with acoustic shadowing was seen in the proximal ureter
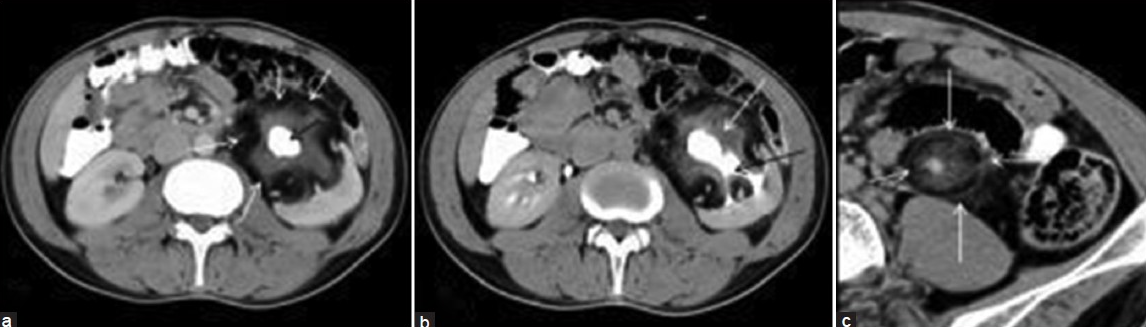
- Axial contrast-enhanced computed tomography (CT) scan showing (a) calculus (black arrow) in left renal pelvis and peripheral fat-attenuating rim (white arrows). (b) The left kidney shows normal enhancement with enhancing periureteric soft tissue (white arrow) and contrast excretion (black arrow) into the calyces. (c) Zoomed-up axial CT images showing the proximal ureteric wall thickening, enhancement and periureteric stranding (white arrows)
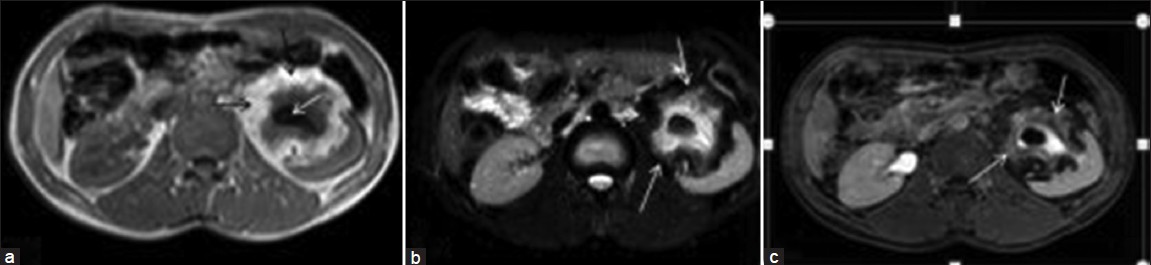
- (a) T1 weighted axial magnetic resonance (MR) image showing calculus in left renal pelvis as a signal void (white arrow) in the centre and a peripheral hyperintense rim of fat (black arrows). (b) Fat sat T2 weighted sequence showing suppression of fat signal (white arrows) and periureteric stranding (c) Axial contrast-enhanced MR T1 images showing enhancing granulation tissue (white arrows) which is isointense and hyperintense on T1 and T2, respectively
The patient underwent left nephroureterectomy. Histopathological report was xanthogranulomatous pyelouretritis. Microscopic examination showed abundance of lipid-laden macrophages, lymphocytes, and plasma cells [Figure 4]. The renal parenchyma was unaffected.
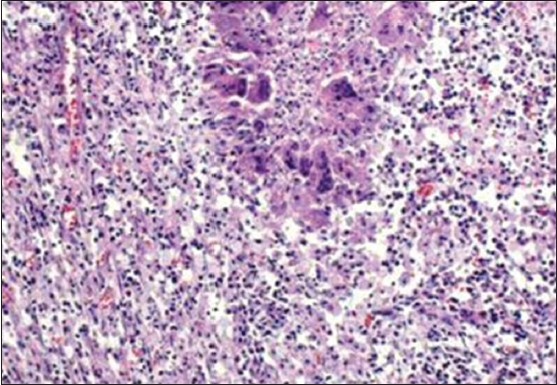
- Microscopic examination showing lymphoplasmocytic infiltration, large foamy (lipid-containing) macrophages and multinuclear giant cells and central necrosis (H and E, ×100)
Xanthogranulomatous pyelouretritis is an extremely rare entity with only two cases described in the literature.[12] The renal parenchyma is normal in morphology and function in xanthogranulomatous pyelouretritis. Lipid-laden macrophage and inflammatory process is confined to the renal pelvis and ureter.[1]
Differentiation of xanthogranulomatous pyelouretritis from xanthogranulomatous pyelonephritis (XGP) may be difficult. Once the diagnosis is confirmed, the goal is to remove all the involved granulomatous tissue. If this is not accomplished, the remaining infected tissue may lead to formation of cutaneous fistulae. When the disease is confined to the ureter, partial ureterectomy is performed. When the process involves the kidneys, partial or total nephroureterectomy is performed according to the severity of involvement.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Ureteral involvement in xanthogranulomatous pyelonephritis - Rare manifestation. Indian J Radiol Imaging. 2006;16:243-5.
- [Google Scholar]






