Translate this page into:
Urinothorax in a Late Kidney Transplant Following Graft Biopsy
Corresponding author: Sukhwinder Singh Sangha, Department of Nephrology, Command Hospital, Panchkula, Haryana, India. E-mail: drsukhi_sangha@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Ghosh I, Sangha SS, Saxena P, Kumar N. Urinothorax in a Late Kidney Transplant Following Graft Biopsy. Indian J Nephrol. doi: 10.25259/IJN_472_2024
Dear Editor,
A 33-year-old male underwent kidney transplant in August 2019. In Jan 2020, he developed graft dysfunction (serum creatinine 2 mg/dL). A biopsy showed borderline T-cell-mediated rejection. He received steroids, augmentation of baseline immunosuppression, and showed good recovery. In May 2022, he presented with bilateral hydrocele, dry cough, mild pain, and swelling at the graft site. Investigations revealed serum creatinine of 2.3 mg/dL and massive right-sided pleural effusion needing intercostal drainage. The fluid was transudative, sterile, and negative for malignant cells. The echocardiogram and spleno-portal doppler was normal. Proteinuria was absent. A pleural fluid-to-serum creatinine ratio of 2.32 favored urinothorax (UT). A radionuclear renogram identified and diagnosed a urine leak [Figure 1]. This was likely secondary to a previous graft kidney biopsy 2 years and 4 months ago. He underwent Foley catheter insertion, double J stenting, and intercostal drainage. His UT gradually improved and serum creatinine settled to 1.5-1.6 mg/dL over 2 months.
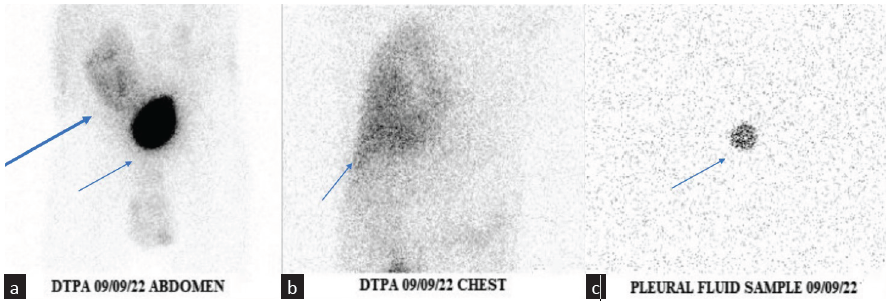
- (a) The thick blue arrow - transplanted kidney with urinary leak. The thin blue arrow - urinary bladder with intense activity indirectly showing the functional status of the transplanted kidney. (b) The accumulation of activity in the right hemithorax (blue arrow). (c) Sample from the pleural fluid showing the presence of activity (blue arrow). DTPA: Diethylenetriamine pentaacetate.
UT is the collection of urine in pleural space resulting from trauma, obstruction, or urinary tract surgery.1 Mechanism of transudation of fluid from the abdominal cavity to pleural space involves diaphragmatic defects. It may happen through lymphatic channels augmented by increased intrabdominal pressure.2 Color and smell of urine, transudative fluid, cellularity, pH, and lactate dehydrogenase are not specific markers of UT.1 Pleural fluid to serum creatinine ratio >1 has a high sensitivity for diagnosing UT. Management includes treatment of underlying cause with drainage of pleural fluid. Pleurodesis may be required.
Following renal transplant surgery, urine leaks are the most common urological complication (10% of cases).3 Urine leaks usually occur at the site of the ureter vesical junction due to necrosis of the distal ureter in the first few weeks of transplant.4 UT following kidney biopsy has not been described in literature.
References
- Urinothorax: A systematic review. J Thorac Dis. 2017;9:1209-18.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Urinothorax: Report of 4 cases and review of the literature. J Urol. 1986;135:805-8.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of urinary fistula after kidney transplantation. Transplant Proc. 2009;41:1624-6.
- [CrossRef] [PubMed] [Google Scholar]
- Perirenal transplant fluid collections. Semin Intervent Radiol. 2004;21:235-7.
- [CrossRef] [PubMed] [Google Scholar]







