Translate this page into:
Xanthogranulomatous Pyelonephritis: Intrahepatic and Intrathoracic Extension
Address for correspondence: Dr. U. Anandh, Department of Nephrology, Yashoda Hospitals, Alexander Road, Secunderabad - 500 003, Telangana, India. E-mail: uanandh@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A 32-year-old female presented to us with worsening cough and expectoration, low-grade fever, and malaise for 3 months. She gave a history of pregnancy loss secondary to urinary tract infection (UTI) a year back. At that time, she was told to have an obstructive right renal calculus. She also had a history of recurrent UTI in the past 1 year. She had no other comorbidities. Her clinical evaluation revealed an enlarged right kidney and reduced air entry in the right hemithorax. Radiological investigations revealed a large right kidney invading into the inferior surface of the right lobe of the liver and the right pleural space. A clinical diagnosis of xanthogranulomatous pyelonephritis was made, and she was advised nephrectomy. Intraoperatively, the right kidney was found to invade both the right lobe of the liver and the right pleural cavity through a right diaphragmatic defect. Histopathology of the kidney revealed the presence of foamy histiocytes suggestive of xanthogranulomatous pyelonephritis. Invasive xanthogranulomatous pyelonephritis is known, however, invasion into the extra-abdominal structures has not been reported in the literature. Our case is a rare manifestation of a rare clinical entity – xanthogranulomatous pyelonephritis.
Keywords
Foamy histiocytes
invasive
renal calculus
urinary tract infection
xanthogranulomatous pyelonephritis
Introduction
Upper urinary tract infection (UTI) in an obstructed kidney, if left untreated, can develop into a chronic destructive granulomatous inflammatory condition known as xanthogranulomatous pyelonephritis.[1] They often present with constitutional symptoms of low-grade fever, weakness, and weight loss.[2] The disease is progressive and in rare instances, the nonfunctional kidney is known to invade surrounding intraabdominal structures. We present an unusual case of xanthogranulomatous pyelonephritis in a young female which not only invaded into the right lobe of the liver but also manifested with respiratory symptoms secondary to an intrathoracic extension.
Case Report
A 32-year-old female with no comorbidities presented to us with a history of a cough with expectoration of 1-month duration. The intensity of cough has been increasing in intensity over the last 1 month. She also has a history of low-grade fever, malaise, and easy fatiguability of the same duration. There was a history of right flank pain and dysuria accompanying her respiratory symptoms.
Her medical history relevant to this illness started 1 year back when she had fever and lower urinary tract symptoms during the second trimester of her second pregnancy. On evaluation, she was told to have UTI and was treated with oral antibiotics. Despite treatment, she lost her baby owing to spontaneous abortion in the 5th month of her pregnancy. She gave a history of 2–3 episodes of UTI following her pregnancy in the past 1 year. All these episodes were managed with oral antibiotics. She gave a history of 20 kg weight loss during the past 1 year.
On clinical evaluation, she was found to have fever, pallor, and mild pedal edema. Her systemic examination revealed a palpable lump in the right lumbar region and reduced breath sounds at the right infrascapular area. Her initial investigations are shown in Table 1. Cultures of the urine and sputum grew the same organism (Proteus mirabilis which was sensitive to cephalosporins, quinolones, aminoglycosides, and carbapenems). The similar sensitivity of the bacterial isolate from the urine and the sputum made us suspect a single source (most probably urinary). She was started on appropriate intravenous antibiotics.

Her computed tomography of the abdomen and chest revealed a grossly enlarged right kidney with obstructive renal calculi. There was a breach on the upper aspect of the kidney suggestive of a ruptured abscess with perinephric extension [Figure 1]. The ruptured abscess was found to be indenting into the lower surface of the right lobe of liver with parenchymal invasion [Figure 2]. The ruptured abscess was also seen to have an intrathoracic extension [Figure 3a and b]. A urology opinion was taken, and after a DTPA scan which showed a completely nonfunctional right kidney, she was advised nephrectomy.

- Grossly enlarged right kidney with obstructive renal calculi

- The enlarged kidney invading into the inferior surface of liver

- (a) Intrathoracic extension of the right kidney. (b) Ruptured abscess extending into the right hemithorax
The patient underwent total nephrectomy; intraoperatively, there was an enlarged right kidney which measured 12 cm × 8 cm × 6 cm with a bosselated external surface [Figure 4]. Cut section showed dilated calyces filled with purulent and yellowish mucoid material. Certain areas of the kidney, especially the lower pole had yellowish discoloration [Figure 5]. Intraoperatively, the retroperitoneal space revealed edematous perinephric tissue. There was a large defect on the inferior surface of the liver [Figure 6]. Pus flecks were seen on the inferior surface of the right lobe of the liver. Above the liver, another large defect was seen in the right hemidiaphragm with pus collection in the pleural cavity [Figure 7]. The microscopic examination of the nephrectomy specimen revealed the presence of lipid-laden foamy macrophages and few giant cells suggestive of xanthogranulomatous pyelonephritis [Figure 8]. These cells stained positive with CD68 on routine immunohistochemistry. There was no evidence of monoclonal staining.
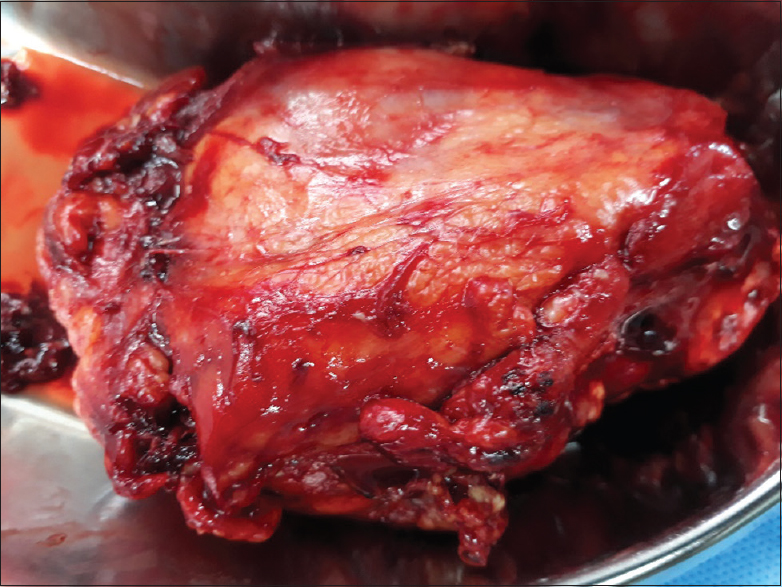
- Nephrectomy specimen

- Gross cut section showing extensive necrosis and yellowish discouloration of the kidney a predominantly at the lower poles
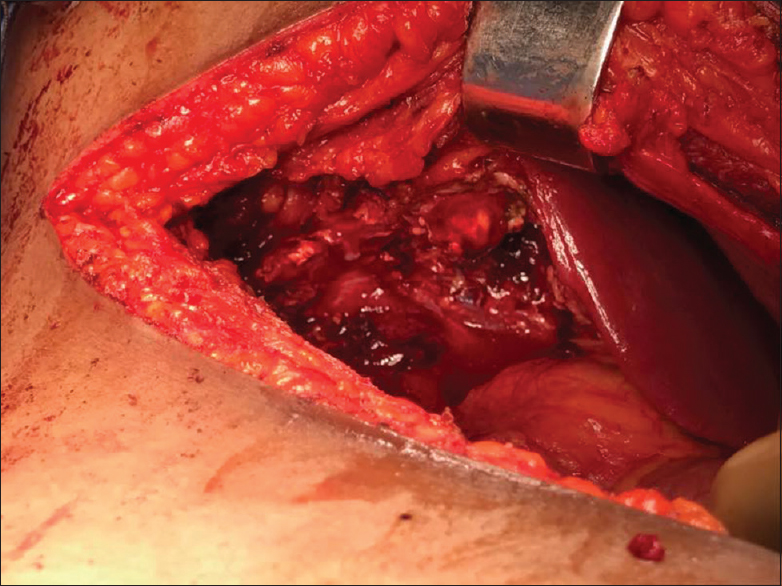
- Defect in the inferior surface of the liver

- Diaphragmatic defect as noted intraoperatively
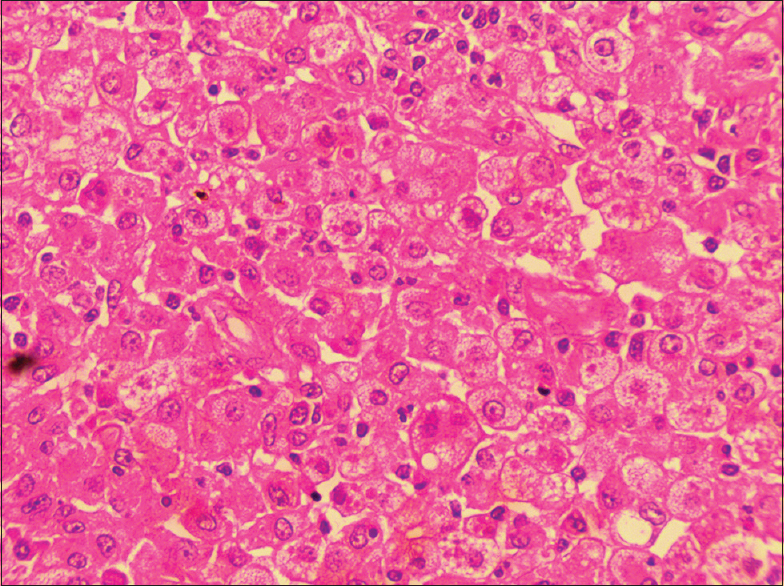
- Histopathology showing numerous lipid-laden foamy histiocytes
The patient underwent a nephrectomy, extensive toileting of the perinephric and infrahepatic space, external drainage of the collected intraabdominal pus, and closure of the right diaphragmatic defect. She was discharged on the 7th post-operative day in a stable condition. On follow-up after a month, she is afebrile, gaining weight, and doing well.
Discussion
Xanthogranulomatous pyelonephritis is a rare entity seen in about 1% of acute pyelonephritis and is usually seen in patients with recurrent UTI with obstructive renal calculi.[3] This entity was first described by Schlangenhaufer.[4] The gross manifestation of this clinical entity is either diffuse or focal and often mimics neoplastic conditions of the kidney from which it should be clinically and pathologically differentiated.[5] Grossly, the kidney is enlarged and often there is evidence of ureteral obstruction (calculi, strictures, etc.). Single or multiple yellowish nodules are noted. Central necrosis and abscess formation are common as was seen in our patient. Perinephric extension as noted in our case is seen in severe cases.[6] Histopathologically, the kidney manifests with sheets of lipid-laden foamy histiocytes. Granuloma formation is seen sometimes.[7] The granulomatous manifestations are seen in sarcoidosis and unusually renal sarcoidosis manifests as xanthogranulomatous pyelonephritis.[8] These xanthomatous histiocytes are positive for CD 68, unlike renal cell carcinoma cells which stain positive for CD 10.[8] Three stages of xanthogranulomatous pyelonephritis have been proposed as follows: Stage I – the lesion is confined to the renal parenchyma, Stage II – the lesion involves the perirenal space, and Stage III – the lesion extends to the pararenal spaces.[5]
Extension beyond the pararenal space is reported rarely into the adjacent organs of adrenals, colon, pancreas, and the abdominal wall. In such clinical situations, they can present with intestinal obstruction, ischemic colitis, pyelocutaneous, and renocolic fistulae.[291011] Xanthogranulomatous pyelonephritis has various other atypical presentation. Occasionally, it mimics as renal cell carcinoma.[12] Extensive abscess formation, destructive invasion into the liver and the right hemithorax is an extremely rare complication and not yet reported in the literature. Ours is the first case in the literature of xanthogranulomatous pyelonephritis presenting with invasion into extra-abdominal organs.
Conclusions
Xanthogranulomatous pyelonephritis is an extremely rare form of pyelonephritis which has a predilection of invading into the adjacent pararenal space and organs. Invasive extension into liver and the thoracic cavity is not yet reported in the literature.
We present an unusual clinical presentation of xanthogranulomatous pyelonephritis which was successfully treated with nephrectomy, drainage of pus, and closure of the diaphragmatic defect.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has/given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initial will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Xanthogranulomatous pyelonephritis: A retrospective study of 10 cases and review of the literature. Saudi J Kidney Dis Transpl. 2001;12:520-4.
- [Google Scholar]
- Xanthogranulomatous pyelonephritis: Clinical findings and surgical considerations. Urology. 1994;43:295-9.
- [Google Scholar]
- Uber eingentumiche staphylomykosen der nieren and des pararennalen bindewebes. Frankf Z Pathol. 1916;19:139-48.
- [Google Scholar]
- Xanthogranulomatous pyelonephritis: A critical analysis of 26 cases and of the literature. J Urol. 1978;119:589-93.
- [Google Scholar]
- Xanthogranulomatous pyelonephritis: A pathological, clinical and aetiological analysis of 87 cases. Diagn Histopathol. 1983;6:203-19.
- [Google Scholar]
- Renal sarcoidosis mimicking xanthogranulomatous pyelonephritis. Urology. 2016;97:e19-e20.
- [Google Scholar]
- Xanthogranulomatous pyelonephritis. A reappraisal and immunohistochemical study. Arch Pathol Lab Med. 1988;112:275-81.
- [Google Scholar]
- Ischemic colitis secondary to xanthogranulomatous pyelonephritis. Int J Infect Dis. 2009;13:e89-91.
- [Google Scholar]
- Xanthogranulomatous pyelonephritis: Detailed analysis of 29 cases and a brief discussion of atypical presentations. J Urol. 1981;126:437-42.
- [Google Scholar]
- Adolescent xanthogranulomatous pyelonephritis mimicking renal cell carcinoma on urine cytology: An atypical presentation. Urology. 2013;81:885-7.
- [Google Scholar]







