Translate this page into:
A Rare Case of Acute Kidney Injury with Central Nervous System Manifestations
Address for correspondence: Dr. Sree Bhushan Raju D, Professor and Head, Department of Nephrology, NIMS, Hyderabad, Telangana - 500 082, India. E-mail: sreebhushan@hotmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Multiple myeloma (MM) is usually a disease of the elderly and only less than 1% are young individuals below 35 years of age. Central nervous system (CNS) manifestations of MM are even rarer, the most common being leptomeningeal involvement. We report a case of a 35-year-old male who presented with a fever of 3 weeks duration associated with slurring of speech, nasal regurgitation, hearing loss, and decreased urine output. CNS examination showed IX, X, and XII cranial nerve palsies with right otitis media and bilateral mastoiditis with conductive hearing loss. Renal biopsy showed cast nephropathy. The kappa–lambda ratio was 18, with β2 microglobulin measuring 12 mg/L. Bone marrow showed 90% plasma cells, and skeletal survey had bony lytic lesions. He responded well to dexamethasone, bortezomib, and thalidomide. His renal functions returned to normal, and palsies have improved completely. This report shows that MM should be suspected even in young patients with classical features of myeloma and CNS involvement is very rare in MM.
Keywords
CNS Involvement
multiple myeloma
young myeloma
Introduction
Multiple myeloma (MM) is a neoplastic plasma cell disorder that is characterized by clonal proliferation of malignant plasma cells in the bone marrow microenvironment, monoclonal protein in the blood or urine, and associated organ dysfunction. The median age at diagnosis is approximately 70 years.[1] Less than 2% of patients are younger than 40 years of age at diagnosis, and it is extremely rare in those younger than 30 years.[2] We report a case of MM in a young patient aged 35 years, who presented to us with unusual neurological manifestations.
Case Report
A 35-year-old man presented with a fever of 3 weeks duration that was low grade, not associated with chills and rigors, and with no evening rise of temperature. He developed slurring of speech with gait instability and impaired hearing, followed by decreased urine output for 2 days. He complained of a holocranial headache associated with vomiting. There was no history of seizures. He was conscious and oriented with no loss of higher mental functions. He did not complain of a decrease in vision or loss of smell. Ptosis was not seen, and corneal and accommodation reflexes were intact. He could perceive the sensation all over the face, and no facial deviation was noted. Along with slurring of speech, the patient had difficulty in swallowing food (liquids > solids), and there was also a nasal voice with nasal regurgitation of food. However, he did not have difficulty in chewing food. There was no head tilt. No focal neurological deficit was noted. On evaluation, there was drooping of the soft palate on the right side. Palatal reflex was sluggish on the right side, with elevation toward the left side. He was able to protrude his tongue outside the mouth, and there was a slight deviation of the tongue tip toward the left side. The jaw jerk was normal, and there was no loss of taste. There was no motor or sensory deficit, and all reflexes were normal. A diagnosis of palsies of the right side IX, X, and XII cranial nerves and conductive-type hearing loss on both sides (right ear more than left) was made. Laboratory examination revealed anemia (hemoglobin level 10.8 g/dL) and hypercalcemia (serum calcium 12.2 mg/dL). His renal function was altered with a serum creatinine of 5.8 mg/dL. He developed paroxysmal supraventricular tachycardia during the hospital stay, which was reverted with adenosine and diltiazem. His magnetic resonance imaging evaluation showed normal brain parenchyma with bilateral mastoiditis [Figure 1]. Contrast was not given in view of renal dysfunction. Cerebrospinal fluid (CSF) analysis showed 10 cells (all lymphocytes) and 60 mg/dL of protein. The rest of the workup was negative. A possibility of tuberculosis involving the central nervous system (CNS) and myeloma involving the brain were suspected. All viral markers (human immunodeficiency virus, hepatitis B virus, and hepatitis C virus) were negative. Further workup showed increased serum protein (10.8 g/dl with globulins 7.6 g/dl) and IgG levels of 5,570 g/dl. Serum protein electrophoresis (SPEP) showed M (monoclonal) spike in the gamma region, and urine Bence–Jones protein (BJP) was absent [Figure 2]. Immunofixation electrophoresis showed lambda restriction, and there were lytic lesions on skeletal survey [Figure 3]. Paraneoplastic etiology workup was done with computed tomography (CT) chest and abdomen [Figure 4]. In the chest, there were bony protrusions in the lower part of the sternum and along the ribs and subpleural nodules in both lungs. Bone biopsy was attempted from the bony protrusion, but a proper sample was not obtained. CT-guided fine-needle aspiration cytology of subpleural nodule was planned, but after discussion with the radiologist, it was deferred in view of high risk of pneumothorax. Cryoglobulins were not evaluated, and there was no abnormal clotting of samples sent at room temperature. There was no evidence of rhabdomyolysis – Creatinine Phospho Kinase (CPK) was not elevated. He had hyperuricemia (Uric acid (UA) 16.5 mg/dL), hyperphosphatemia (Phosphorus (iPO4) 9.2 mg/dL), hypokalemia, and hypercalcemia. Antineutrophil cytoplasmic antibody was negative. Bone marrow showed 90% plasma cells. He was initially treated for mastoiditis and started on tablet dexamethasone, injection bortezomib, and tablet thalidomide, which led to resolution of renal dysfunction (serum creatinine 1.6 with improved palsies). Six months after the treatment, he was found to have no abnormality in cranial nerves and had normal renal function tests.
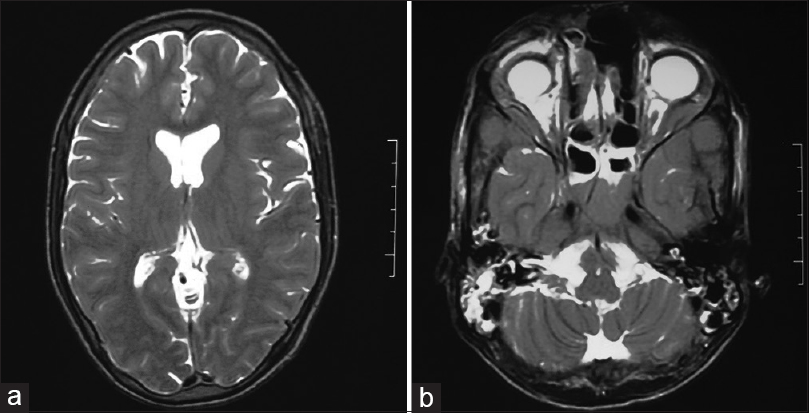
- (a) MRI brain with normal parenchyma, (b) MRI Brain with bilateral mastoiditis
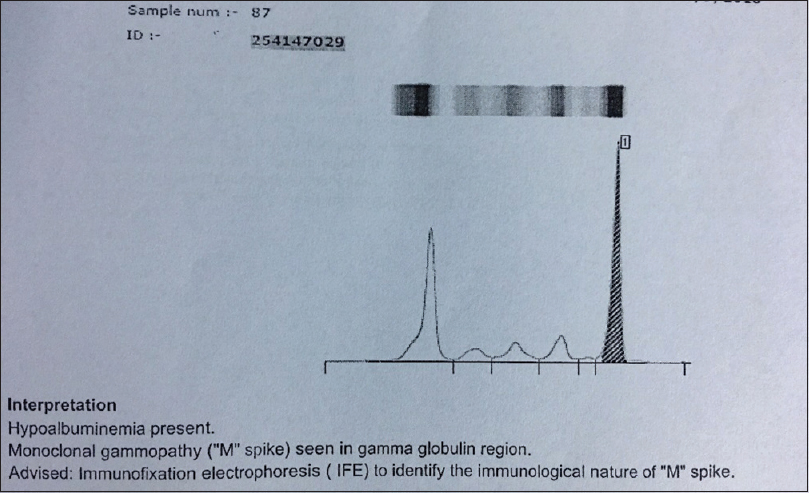
- SPEP showing M spike in gamma globulin region
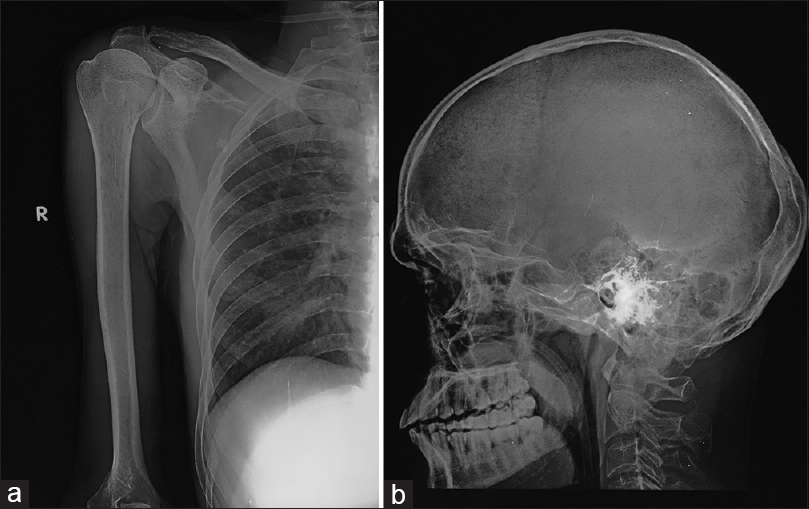
- (a) Upper end of humerus right side showing lytic lesion, (b) X-Ray lateral view skull

- HRCT chest showing bony protrusion from lower end of sternum
Discussion
MM is a malignant disorder that is characterized by the proliferation of monoclonal plasma cells.[2] The peak incidence of MM is in the seventh decade, whereas it is a rare entity in young patients, with less than 2% cases occurring in patients younger than 40 years of age, and it is still rarer in patients who are younger than 30 years.[3] In a study by National Cancer Institute, the frequency of such occurrence was seven out of 3,815 (0.18%).[4] Hewell and Alexanian[5] have reported a frequency of 1%. These patients were thefirst well-documented group of young persons with MM. The records of all patients younger than 30 years with MM evaluated at the Mayo Clinic were reviewed and the incidence was found to be 0.3%.[2] Goel et al.[6] found from a study in Manipal that seven out of 87 patients with MM were young. MM in the young has an atypical clinical presentation with multiple or solitary extramedullary plasmacytoma and osteolytic lesions, but low serum or urinary monoclonal M proteins and few or no plasma cells in the bone marrow.[25] The clinical behavior of MM in adolescents and young adults has been suggested to be more indolent.[78] Our patient was a 35-year-old male with atypical presentation. He had acute kidney injury (AKI) with lower motor-type cranial palsies. The presentation was suggestive of infective etiology other than MM, but the laboratory evaluation suggested classical features of anemia, hypercalcemia, renal dysfunction, and M spike on SPEP. He did have multiple bony lesions and subpleural nodules suggestive of plasmacytoma, but it could not be proved histologically. Renal function impairment is a well-known complication of MM. A Mayo Clinic analysis revealed renal function impairment and hypercalcemia in 30% and 20% of the patients, respectively.[2] In our patient, there was evidence of hypercalcemia and renal impairment requiring dialysis. Lazarus et al.[8] reported two cases of plasma cell myeloma in young patients. One was a case of MM involving the skull and ribs in a 23-year-old woman and the other was solitary myeloma of the tibia in a 21-year-old man. Both cases were diagnosed as nonsecretory MM. However, monoclonal Ig was demonstrated by immunohistochemical studies. In our subject, there was a beta-2 peak in the SPEP. The immunohistochemical examination demonstrated a strong reaction for the lambda light chain in all tumor cells with a positive BJP in urine. However, only the report by Bladé et al.[2] found BJP in five out of 10 patients. The literature review suggests that there may be an associated extramedullary component in most of these patients. Geetha et al.[9] from India described two young patients (20 and 18 years, respectively) who presented with extradural cord compression, lytic bone lesions, and bone marrow plasmacytosis. In our subject, there was definite extramedullary involvement in the form of cranial nerve palsies and plasmacytomas.
CNS involvement in MM in a case series reported by Schluterman showed four of 23 patients with multiple cranial nerve palsies.[10] Leptomeningeal meningitis (LMM) was the most common presentation, with CSF analysis showing increased pleocytosis and proteins. Marjanović et al.[11] showed that CSF IgG levels to serum albumin levels can be used to determine CNS LMM involvement. A case report showed the presentation of acute vision loss with multiple brain parenchymal plasmacytomas.[12] The prognosis was poor and the patient expired. CNS involvement of MM portends a poor prognosis.
Although our patient had a severe presentation with AKI and CNS involvement, the diagnosis was swift and treatment was initiated after treating mastoiditis. He received standard injection dexamethasone, injection bortezomib, and tablet thalidomide. The response was good, and his AKI that required only one session of hemodialysis resolved completely. He received six cycles of the cyclophosphamide, bortezomib, and dexamethasone (CyBorD) regimen, and recovered fully and attained complete remission at the end of 6 months. His cranial nerve palsies also recovered completely with no residual deficit. The median duration of survival of patients with MM ranges between 2 and 3 years. In the study from Mayo Clinic, the median duration of survival of the patients was 87 months. The survival of the younger patients was considerably longer than that of patients of all ages with MM.[5] These results support the beneficial effect of a high index of suspicion and early diagnosis of patients at young age with MM.
Our patient was young with acute presentation suggesting a good prognosis and CNS symptoms heralding a poor prognosis; he recovered fully.
Conclusion
In conclusion, this report illustrates that MM should be suspected in young patients, on appropriate clinical grounds, especially if there are suggestive biological or radiological signs. CNS involvement is rare with lower motor neuron involvement being the most common.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Multiple myeloma in patients younger than 30 years. Report of 10 cases and review of the literature. Arch Intern Med. 1996;156:1463-8.
- [Google Scholar]
- Plasma cell myeloma in unusually young patients: A report of two cases and review of the literature. Skeletal Radiol. 1995;24:47-51.
- [Google Scholar]
- Presenting features and prognosis in 72 patients with multiple myeloma who were younger than 40 years. Br J Haematol. 1996;93:345-51.
- [Google Scholar]
- Plasma cell dyscrasia in a 15-year-old boy: Case report and review of the literature. Am J Med. 1990;89:816-8.
- [Google Scholar]
- Multiple myeloma in young men. Clinical course and electron microscopic studies of bone marrow plasma cells. Cancer. 1980;46:1397-400.
- [Google Scholar]
- Multiple myeloma invasion of the central nervous system. Arch Neurol. 2004;61:1423-9.
- [Google Scholar]
- Multiple myeloma invasion of the central nervous system. Vojnosanit Pregl. 2012;69:209-13.
- [Google Scholar]
- Acute vision loss revealing central nervous system aggressive myelomatosis. J Neurol. 2012;259:2749-51.
- [Google Scholar]







