Translate this page into:
A Rare Case of Bilateral Renal Abscess from Staphylococcal Infection in a Young Healthy Patient
Address for correspondence: Dr. Atthaphong Phongphithakchai, Division of Nephrology, Department of Internal Medicine, Faculty of Medicine, Prince of Songkla University, 15 Kanchanavanit Road, Hat Yai, Songkhla 90110, Thailand. E-mail: ton331@hotmail.com, patthaph@medicine.psu.ac.th
-
Received: ,
Accepted: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Bilateral renal abscess is a rare infectious disease. Most patients have some risk factors for comorbidities, such as diabetes or an abnormal urinary tract, causing abscess formation. The incidence of the disease is infrequent in young healthy adults. Here, we report a case of a previously healthy non-diabetic young man who presented with abdominal pain with a high-grade fever. With clinically persistent abdominal pain, computerized tomography of the whole abdomen was done. The result showed bilateral renal abscess. The culture from the abscess reported Staphylococcus aureus. The patient’s clinical abdominal pain and fever resolved after receiving antibiotics for 4 weeks.
Keywords
Bilateral renal abscess
computed tomography
healthy
percutaneous drainage
Introduction
Renal abscess is a rare disease with an incidence of 0.2% among the various types of intra-abdominal abscess.[1] Abscesses usually occur in patients with predisposing systemic conditions, such as diabetes mellitus liver cirrhosis,[2] or abnormalities of the urinary tract.[2] Other less common risk factors are intravenous drug abuse and chronic debilitating disease. Because the clinical features are non-specific treatment gets delayed leading to increased mortality and morbidity, especially in patients with advanced age and lethargy.[3] It is rare to find renal abscesses in young adults without predisposing factors. We report an unusual case of bilateral renal abscess in a young healthy patient.
Case Report
A 23-year-old male was admitted to Songklanagarind Hospital, a tertiary hospital in southern Thailand, on 12 October 2021 with a high-grade fever for two days. One week prior to admission, he had abdominal pain on the upper right side. The characteristic of the pain was dull aching. The duration of pain was 10 minutes each time, about 10 times a day. He did not complain of dysuria or icteric sclera. He began to have a fever with chills and anorexia 5 days later. He took acetaminophen to relieve the symptoms, but it was ineffective. Then, he went to the hospital. He denied having any underlying medical conditions. He denied a history of congenital abnormalities of the urogenital system, unprotected sexual behaviour, or injected drug use. His alcohol consumption was one bottle per week. He had no previous surgical history.
On examination, he was drowsy and febrile. The pulse was regular at 96 per minute, and his respiratory rate was 20 per minute. His blood pressure was 112/58 mm Hg. The oxygen saturation was 98%. He had anicteric sclera and no pale conjunctiva. The respiratory and cardiovascular examination did not show any abnormalities. On abdominal examination, he was tender on the right upper quadrant of the abdomen and right costovertebral area. The bimanual palpation was negative. The urinary bladder could not be palpated.
Laboratory investigation revealed anaemia (haemoglobin 11.9 g/dl), leukocytosis (white blood cell 16,800 with PMN 81.8%,), but no thrombocytopenia. Liver function tests showed mild transaminitis with aspartate transaminase of 54 U/L and alanine transaminase of 60 U/L. The total bilirubin was 1.37. The patient’s serum creatinine was 1.1 mg/dl and blood urea nitrogen was 12.7 mg/dl. Urinary analysis showed no proteinuria or cells. Blood sugar was normal. The enzyme-linked immunosorbent assay for human immunodeficiency virus was negative. The serological screening for hepatitis B and hepatitis C were negative.
Computerized tomography (CT) abdomen showed two defined enhancing multiloculated cyst lesions about 4.7 × 3.8 cm and 3.6 × 3.2 cm at lower poles of right and left kidney with surrounding bilateral perinephric fat stranding and minimal perirenal fluid as well as thickening of bilateral Gerota’s and Zunckerkandl’s fascia [Figure 1]. There were no stones, hydronephrosis, or hydroureter. The rest of the liver and biliary tract appeared to be normal. Multiple rounds non enhancing nodules up to 1 cm at the posterior and lateral basal segment of the right lower lung and lateral segment right middle lung were observed.

- Contrast-enhanced computerized tomography imaging of the abdomen (a) two defined enhancing multiloculated cyst lesions on the lower poles of the right and left kidney (arrows). (b) resolving two cyst lesions of both kidneys after treatment for 4 weeks
Based on the clinical manifestations and CT abdomen findings of multiloculated cyst lesions on both kidneys, the patient was diagnosed with a bilateral renal abscess. The haemoculture and urine culture found no organisms. The patient underwent ultrasound-guided percutaneous drainage of the abscess in the right kidney [Figure 2]. The aspirated pus was sent for culture to identify the causative organism, which revealed numerous colonies of methicillin-sensitive Staphylococcus aureus (MSSA) [Figure 3]. The transesophageal echocardiogram did not show any vegetation.
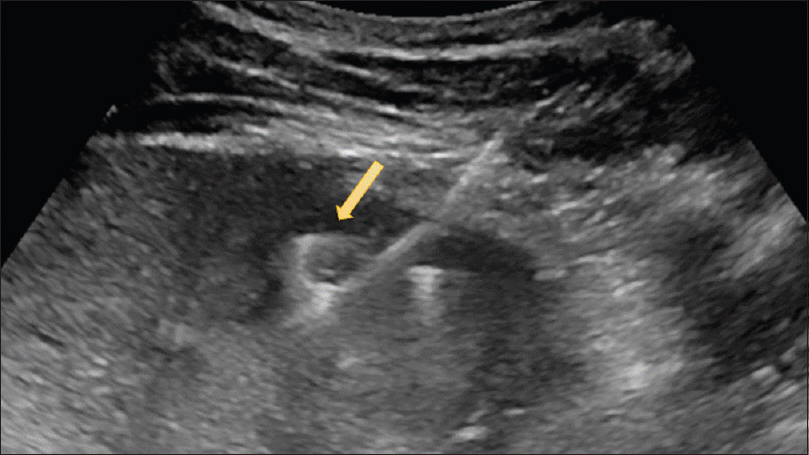
- Ultrasound-guided percutaneous drainage showing the pigtail catheter advanced into the hypoechoic portion of the right renal abscess (arrow)
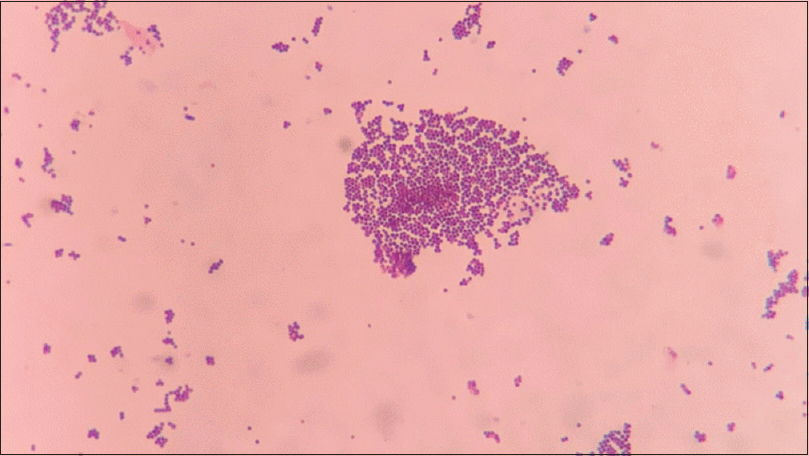
- Gram stain of a colony showing Gram-positive cocci in clusters, compatible with Staphylococcus aureus
The patient was given empirical parenteral ceftriaxone for two weeks and was then switched to cefazoline after drug susceptibility cultures were reported. The total duration of antibiotic treatment was four weeks. On the seventh day of treatment, the patient’s symptoms had improved. His fever had subsided, his appetite had improved, and he had gained weight and did not complain of abdominal pain. The complete blood count revealed no leukocytosis with stable renal function. An abdominal CT scan was repeated at four weeks and showed considerable improvement of the lesions in both kidneys, which the lesion size has decreased to 0.3×0.1 cm in the right kidney and 0.2×0.1 cm in the left kidney, respectively.
Discussion
The pathogenesis of renal abscess can be divided into two main mechanisms: (1) hematogenous spread from the primary site of infection; this condition is usually Staphylococcus aureus and other Streptococci in patients receiving intravenous injections, especially in patients with drug addiction. Characteristically, the abscess is located predominantly in the renal cortex due to the branching of blood vessels. (2) Ascending infection of the lower urinary tract, typically caused by Gram-negative organisms such as Escherichia coli. These usually occur in cases of urinary tract obstruction or pre-existing abnormality of kidney structure.[4] Our case is a rare occurrence of bilateral renal abscess in a patient without underlying conditions, like previous reports of healthy individuals who presented with bilateral renal abscess.[5]
The clinical presentation is categorized into chronic development and acute condition. In chronic development, the disease is silent and only presents signs and symptoms related to upper urinary tract infection. In contrast, acute conditions from metastatic infection display more severe symptoms, such as high-grade fever and varying levels of flank pain.[6] Some case series have reported non-specific symptoms like undefined abdominal pain or fever of unknown origin.[7] Thus, it is important to perform a careful clinical evaluation to avoid a delay in diagnosis.
Renal imaging is the recommended investigation to establish the diagnosis of a renal abscess. With these modern modalities, mortality has dramatically decreased, and a good prognosis can be expected when the diagnosis is made promptly.[8] First, renal ultrasonography (USG) is widely available, not expensive, and non-invasive. The diagnostic yield is around 70-93%, depending on previous reports.[79] However, there are some limitations to this modality, that is., the size of the renal abscess must be at least 2-3 cm in diameter to detect by USG and could be confused with other lesions such as hematomas or other mass lesions.[7] CT imaging is more accurate and specific than USG, with a diagnostic rate of 96%.[9] This technique can provide better information on abscess size and is better at evaluating perinephric involvement, including the extension of the abscess.[39] The typical finding of renal abscess on CT imaging is a geographic low-attenuation collection with rim enhancement, but no central enhancement.[10]
Early treatment is related to good clinical outcomes. Antibiotics must be started immediately after diagnosis. However, other management choices, such as percutaneous drainage, can be considered in individual cases.[11] The initial empiric antibiotic regimen should have activity against Enterobacteriaceae and Staphylococcal infection, such as fluoroquinolones or penicillinase-resistant penicillin plus an aminoglycoside.[12] In patients with an abscess size <5 cm, antibiotics alone can successfully lead to clinical resolution. However, if the size is ≥5 cm, a drainage manoeuvre is preferred.[13] Some previous retrospective studies have reported comparable outcomes of percutaneous drainage and surgical drainage in large abscesses. Additionally, a larger size is associated with a poor prognosis and treatment outcome.[14] Percutaneous drainage can provide a care rate of 93%.[15] Our case received intravenous broad-spectrum antibiotics and underwent percutaneous drainage of the right renal abscess due to its large size (nearly 5 cm). This provided an advantage in organism identification and increased the resolution rate in conjunction with antibiotics. However, there have been no randomized controlled studies evaluating the effectiveness of drainage methods in patients with varying sizes of the abscess.
In conclusion, this case report describes a young healthy adult who developed a bilateral renal abscess without pre-existing factors. This is a rare condition but must be taken into consideration in healthy individuals presenting with high-grade fever and abdominal pain. Renal imaging modalities such as USG or CT scans are the cornerstone in establishing the diagnosis. Prompt treatment with an empirical intravenous antimicrobial agent is crucial.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
References
- Recent clinical overview of renal and perirenal abscesses in 56 consecutive cases. Korean J Intern Med. 2008;23:140-8.
- [Google Scholar]
- Recent clinical overview of renal and perirenal abscesses in 56 consecutive cases. Korean J Intern Med. 2008;23:140-8.
- [Google Scholar]
- An unexpected case of bilateral kidneys studded with multiple abscesses, in a nondiabetic healthy woman-A case report. Asian J Med Sci. 2014;6:91-3.
- [Google Scholar]
- Renal and perinephric abscesses:Analysis of 65 consecutive cases. World J Surg. 2007;31:431-6.
- [Google Scholar]
- Presentation, diagnosis and treatment of renal abscesses: 1972-1988. J Urol. 1994;151:847-51.
- [Google Scholar]
- Assessment and characterisation of common renal masses with CT and MRI. Insights Imaging. 2011;2:543-56.
- [Google Scholar]
- Current clinical management of renal and perinephric abscesses:A literature review. Urologia. 2014;81:144-7.
- [Google Scholar]
- Edn presented at the EAU Annual Congress Amsterdam, the Netherlands. 2022 ISBN 978-94-92671-16-5
- [Google Scholar]
- Renal abscesses measuring 5 cm or less:Outcome of medical treatment without therapeutic drainage. Yonsei Med J. 2010;51:569-73.
- [Google Scholar]
- Immediate percutaneous drainage compared with surgical drainage of renal abscess. Int Urol Nephrol. 2007;39:51-5.
- [Google Scholar]
- Perinephric abscess as a rare cause of acute abdomen:A case report. J Surg Med. 2020;41:102-4.
- [Google Scholar]







