Translate this page into:
Acute Purulent Pericarditis Caused by Klebsiella Pneumonia in a Patient ESRD on Hemodialysis
Address for correspondence: Dr. K. Vinod Kumar, Aster Medcity, Cheranalloor, Kochi - 682 027, Kerala, India. E-mail: drvinodkumark17@gmail.com
-
Received: ,
Accepted: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Pericardial involvement can be seen in patients with end-stage renal disease (ESRD) undergoing hemodialysis. With improvement in the quality of dialysis, the incidence of pericarditis has come down to less than 5%.[1] Purulent pericarditis is usually caused by gram-positive organisms such as Staphylococcus spp. However, the spectrum of causative organisms is changing in recent times.[2]
Here we report a 30-year-old male kidney transplant recipient who presented to us with a history of nonproductive cough, breathlessness, and fatigue of 1-week duration. He was on triple immunosuppression (tacrolimus, mycophenolate mofetil, and prednisolone). He developed acute antibody-mediated rejection a year later and was treated with intravenous steroids and bortezomib, but there was no response to treatment. Graft function progressively worsened and received maintenance hemodialysis for 2 years through a right brachiocephalic arteriovenous fistula; immunosuppressive medications were stopped and he was continued only on prednisolone 5 mg once daily.
Investigations revealed hemoglobin 8 gm/dl, total leukocyte count 10,000 cells/cumm, C-reactive protein 225 mg/dl, and serum Ferritin levels of 7486 ng/dl (acute phase reactant). Chest radiograph showed cardiomegaly. Echocardiogram confirmed massive pericardial effusion with fibrinous strands within the fluid and no features of pericardial tamponade. Computed tomography (CT) thorax showed a nodular lesion (1.4 × 1 cm) in the right lower lobe of the lung in the anterior basal segment abutting the oblique fissure with central cavitation [Figure 1a] and a large pericardial effusion [Figure 1b]. Culture of the pericardial fluid grew Klebsiella pneumoniae sp. (extended spectrum beta-lactamase producer) which was sensitive to meropenem and amikacin. Tests for tuberculosis (acid-fast bacilli stain, culture, and GeneXpert) were negative.
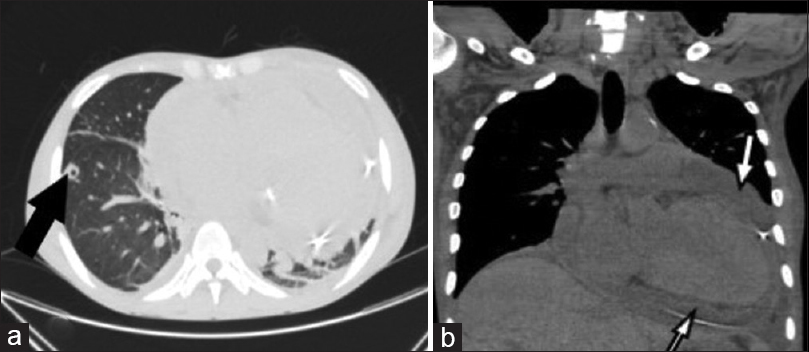
- (a) Computed tomography (CT) thorax shows a nodular lesion in right lower lobe with central cavitation (black arrow) and (b) pericardial effusion (white arrow)
Pericardiocentesis was done and 1500 ml of purulent fluid was drained with markedly elevated leukocyte counts (85,000 cells/cmm) and over 90% neutrophils. A pigtail catheter was placed in the pericardial cavity for continuous drainage. He was started on intravenous meropenem (500 mg twice daily) and amikacin (250 mg once daily). He had persisting fever spikes even after 3 days of intravenous antibiotics and the drain was around 500–700 ml per day. Intrapericardial instillation of amikacin was done for 3 days and intravenous meropenem and amikacin were continued for a total duration of 3 weeks. The pigtail drainage catheter was kept for two weeks. The patient improved symptomatically, and pericardial effusion resolved completely in 4 weeks’ time.
The incidence of pericarditis in maintenance hemodialysis patients is around 5%–20%, mostly due to uremia. Primary bacterial infection of the pericardium is uncommon.[2-4] Although in most cases, classical gram-positive bacteria such as Staphylococcus and Streptococcus are seen, there is an emergence of gram-negative and anaerobes as well.[3,4] In developed countries, viral etiology is common and in the developing countries, Mycobacterium tuberculosis remains prevalent.[3,4] Adjacent infective foci such as pneumonia, pleural empyema, and subdiaphragmatic abscess extending into the pericardium are usually the source, others being hematogenous spread from distant foci or from wounds. Other risk factors for patients to develop Pericarditis include history of thoracic surgery, malignancy, alcohol abuse, and diabetes mellitus.[3] Our case, it is likely that it is an extension of the Klebsiella infection of the lung into the pericardial cavity that caused pericardial effusion.
Muhammed et al.[5] found vancomycin to be an effective agent for intrapericardial antibiotic irrigation for purulent pericarditis caused by Streptococcus sp. There is no data for using other antibiotics for intrapericardial irrigation. In our case, as there was a poor response to intravenous antibiotics initially, we decided to use intrapericardial irrigation with amikacin at a dose of 2 mg/kg daily for 3 days, after which there was a significant reduction in the drain volume and his symptoms. Our patient required prolonged pigtail drainage, dual parenteral antibiotics, and intrapericardial irrigation with amikacin and finally had good resolution of pericardial effusion as well as the lung lesion.
To the best of our knowledge, this is the first case of purulent pericarditis caused by Klebsiella pneumonia reported in a maintenance hemodialysis patient. Pericardiocentesis is useful in large effusions and targeted antibiotics are necessary. Intrapericardial instillation of antibiotics can yield a faster recovery.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Pericardial effusion in patients with end-stage renal disease. Tex Heart Inst J. 2015;42:596-6.
- [Google Scholar]
- Staphylococcal pericarditis in a chronic renal failure patient. Ren Fail. 2003;25:493-8.
- [Google Scholar]
- Post-transplant recurrent pericarditis with pericardial tamponade is successfully treated with colchicine: A case report. Exp Thera Med. 2014;8:801-4.
- [Google Scholar]
- Intrapericardial antibiotic irrigation for purulent pericarditis. Am J Respir Crit Care Med. 2015;191:A1670.
- [Google Scholar]






