Translate this page into:
AL Amyloidosis in a Patient with Long-Standing Rheumatoid Arthritis: Is there a Link with Autoimmune Disease and Monoclonal Gammopathy of Renal Significance?
Address for correspondence: Dr. Urmila Anandh, Department of Nephrology, Yashoda Hospitals, Alexander Road, Secunderabad, Hyderabad - 500 003, Telangana, India. E-mail: uanandh@gmail.com
-
Received: ,
Accepted: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
A variety of kidney leasions are seen in patients with rheumatois arthritis (mesangial glomerulonephritis, IgA nephropathy, membranous nephropathy, etc.), tubulointerstitium (interstitial nephritis), and the vessels (rheumatoid vasculitis).[1] Amyloidosis is also seen in long-standing RA and is often the AA type as described in the literature.[2]
We report a case of a lady with long-standing RA with multiple joint deformities who presented to us with proteinuria and backache. Her investigations revealed anemia (hemoglobin 10.5 g/dl), normal renal functions (creatinine 0.5 mg/dl), and a low serum albumin (3.2 g/dl). The A:G ratio was 0.9. The serum calcium (9.2 mg/dl) and uric acid (5.4 mg/dl) were within normal limits. The urine examination showed 2+ albumin, 2 wbc/hpf, and 13 rbc/hpf. Urine protein creatinine ratio was 1.26. Complement levels were normal, antineutrophilic cytoplasmic antibodies and antinuclear antibodies were negative. The ultrasound of the kidneys revealed normal-sized kidneys. In view of active urinary sediment and subnephrotic proteinuria, she underwent a renal biopsy.
The light microscopy and immunoflorescence study of the biopsy revealed focal glomerular obsolescence (2/8) with mild tubulo-interstitial chronicity (5–10%) and insignificant IgM deposits. The renal biopsy was stained for congo red and SAA protein, both of which came negative. The electron microscopic evaluation revealed mesangial and subepithelial aggregates of randomly oriented fibrillary structures [Figure 1a and b]. These fibrils measured about 9–11.6 nm in diameter (mean fiber diameter 10.4) [Figure 2]. There was no evidence of any electron-dense deposits in GBM or mesangial areas. A pathological diagnosis of Amyloidosis was made.

- (a) Electron micrograph showing subepithelaia and mesangial deposition of amyloid fibrils. (b) Higher magnification of the amyloid fibrils
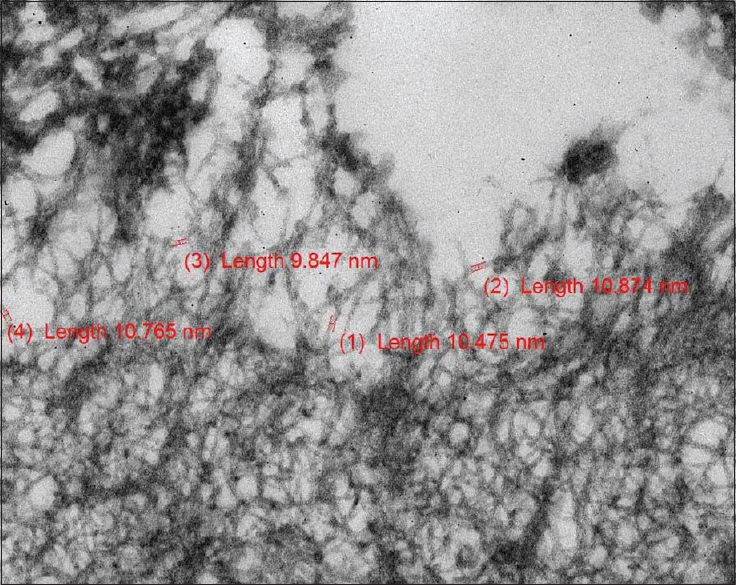
- Amyloid fibrils measured between 9 and 11.6 nm
On further investigations, serum-free light chains assay showed a lambda light chain restriction with the κ/λ ratio of 0.04. (Normal 0.26–1.65). Serum electrophoresis did not reveal a M spike. Because of the hematological findings suggestive of monoclonal gammopathy, a bone marrow biopsy was done which showed the presence of 8–10% plasma cells. Immunophenotyping of the cells showed CD138 positive lambda restricted monoclonal plasma cells. The skeletal survey did not show any lytic lesions.
The final diagnosis was monoclonal gammopathy of renal significance (MGRS) with AL amyloidosis in the renal biopsy. The clinical features did not satisfy the diagnostic criteria of multiple myeloma. She received 24 cycles of bortezomib and dexamethasone. Currently, her κ/λ ratio is within normal limits. Her serum creatinine is 0.6 mg/dl and her protein creatinine ratio is 0.1.
Association between autoimmune disorders and monoclonal gammopathy has been reported sporadically. Kobayashi et al. have reported a case of Sjogren’s syndrome who went on to develop monoclonal gammopathy of undetermined significance (MGUS).[3] Large epidemiological studies have shown association between autoimmune disease and MGUS.[4] However, a recent epidemiological study and a meta-analysis have failed to reveal any association between multiple myeloma and autoimmune diseases.[5,6]
The jury is still out about the link between autoimmune diseases and MGRS. Our case report highlights the presence of AL (not AA) amyloidosis in a patient of RA in this era of therapy with various biologics. Whether long-standing disease modifies the immune system or the drug therapy is responsible for the development of the monoclonal proliferation of plasma cells still remain an open question.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The clinical and pathological characteris ticsof nephropathies in connective tissue diseases in Japan Renal Biopsy Registry (J-RBR)Clin Exp Nephrol. . 2017;21:1024-9.
- [Google Scholar]
- Systemic AA amyloidosis: Epidemiology, diagnosis and management. Clin Epidemiol. 2014;6:369-77.
- [Google Scholar]
- Fanconi's syndrome and distal 9 type 1) renal tubula acidosis in a patient with primary Sjogren's syndrome with monoclonal gammopathy of undetermined significance. Clin Nephrol. 2006;65:427-32.
- [Google Scholar]
- Disease associations with monoclonal gammopathy of undetermined significance: A population based study of 17398 patients. Mayo Clin Proc. 2009;84:685-93.
- [Google Scholar]
- The impact of rheumatological disorders on lymphomas and myeloma: A report on risk and survival from the UK's population-based Haematological Malignancy Research Network. Cancer Epidemiol. 2019;59:236-43.
- [Google Scholar]
- Risk of multiple myeloma in rheumatoid arthritis;A meta-analysis of case-control and cohort studies. PLoS One. 2014;9:e91461.
- [Google Scholar]






