Translate this page into:
Bilateral Renal Cortical Necrosis in a Case of Granulomatosis with Polyangitis
Address for correspondence: Dr. Krishan Lal Gupta, Department of Nephrology, PGIMER, Chandigarh, India. E-mail: klgupta@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Granulomatosis with polyangitis (GPA), previously called as Wegener's granulomatosis, is known to present with necrotizing vasculitis predominantly involving small- and medium-sized vessels. However, isolated renal artery vasculitis without glomerulonephritis leading to cortical necrosis in GPA has not been reported in literature. Here, we describe a case of renal cortical necrosis in a case of GPA.
A 43-year-old female presented to our hospital with history of decreased urine output, fever, and shortness of breath for 2 weeks' duration. She was known to be hypertensive and diabetic for the past 5 years and was on irregular treatment. Her background history was significant in that she was diagnosed as a case of GPA 1.5 years back when she presented with fever and cough. Computed tomography (CT) chest showed multiple thick-walled cavities, antineutrophilic cytoplasmic antibody was negative both by ELISA and indirect immunofluorescence, and renal function was normal with a serum creatinine of 0.9 mg/dL and no active urinary sediments. Positron emission tomography–guided biopsy from the lung cavities revealed granulomatous inflammation with vasculitis. The patient was managed as antineutrophil cytoplasmic antibody (ANCA)-negative GPA and received oral steroids for 6–8 weeks and rituximab induction (375 mg/m2 weekly for four doses). After this induction therapy, the patient was lost to follow-up and presented this time after 18 months with the above complaints. On admission, laboratory parameters revealed hemoglobin of 8.5 g/dL, total leucocyte count of 17,500/mm3, serum creatinine of 9.5 mg/dL, and urinalysis showed no active sediments. Blood and urine cultures were sterile, and ultrasonography revealed normal size kidneys. Antiproteinase 3 antibody was positive by ELISA. Antinuclear antibody, anti-DsDNA, C3, C4, antimyeloperoxidase antibody, anticardiolipin antibody, lupus anticoagulant, hepatitis B serology, and anti-GBM antibody ELISA were negative. The patient was started on hemodialysis, and renal biopsy was performed which showed multifocal cortical necrosis including 70% of the total cortex with ischemic wrinkling of glomerular tuft [Figure 1]. Medium-sized vessel showed evidence of vasculitis with break in internal elastic lamina and recanalized thrombus in the vessel lumen [Figures 2 and 3]. Immunofluorescence was negative for IgG, IgM, IgA, and C3 with overall features suggestive of acute cortical necrosis with arteritis. CT angiography of abdomen revealed no features of renal artery aneurysms or stenosis. In view of possibility of renal relapse of ANCA vasculitis, she was given methylprednisolone pulse 15 mg/kg for 3 days followed by oral steroids at 1 mg/kg and cyclophosphamide pulses as per European vasculitis protocol. Seven sessions of plasmapheresis were also administered. Her urine output gradually improved and the patient became dialysis-independent and afebrile. She was started on azathioprine maintenance after completion of six pulses of cyclophosphamide. At 6 months of follow-up, her serum creatinine is stable at around 2.5–3 mg/dL.

- Low power view of PAS stained renal biopsy showing multifocal cortical necrosis with ghost glomeruli and atrophic tubules with loss of nuclear details
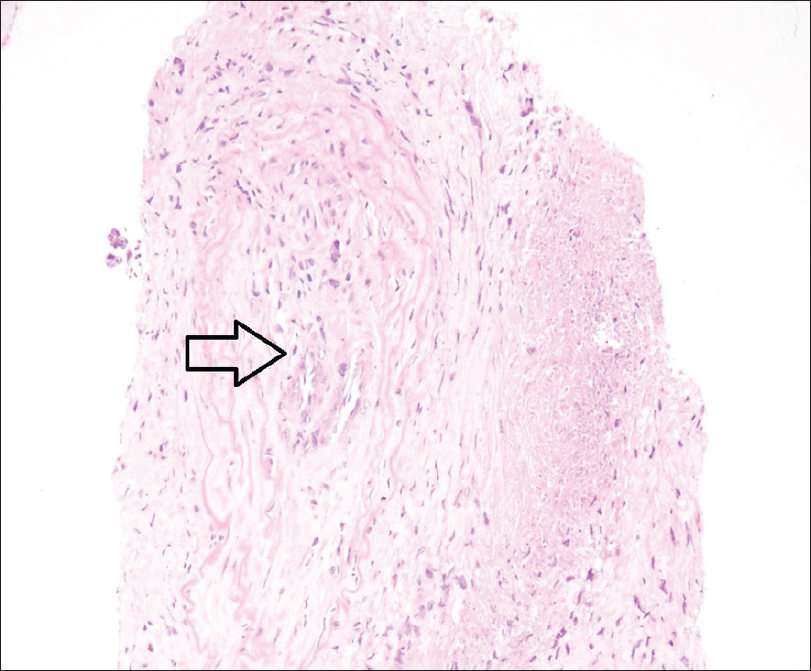
- High power photomicrograph of renal biopsy showing medium sized artery with recanalised thrombus in the lumen and infiltrating polymorphs (arrow)

- High power photomicrograph (elastic Von gossa stain) showing medium sized artery with break in internal elastic lamina suggestive of arteritis
GPA involving the kidneys usually leads to pauci-immune necrotizing glomerulonephritis with crescents.[1] Rarely, thrombotic microangiopathy and suppurative interstitial nephritis have been described in ANCA-associated vasculitis on renal biopsy.[23] We describe a case of GPA with renal relapse which unusually had bilateral renal cortical necrosis with arteritis on histopathology. Acute renal cortical necrosis is caused by obstetrical complications in 60%–70% of cases. The remaining 30%–40% of cases are caused by sepsis, snake bite, and hemolytic uremic syndrome.[4] It has also been reported in antiphospholipid antibody syndrome.[5] However, GPA leading to renal cortical necrosis due to extraglomerular renal arteritis has not been described so far. Hence, we highlight the fact that clinicians should also keep vasculitis as a differential cause of renal cortical necrosis to avoid delay in treatment and organ damage.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Renal involvement in systemic vasculitis. In: Jennette JC, Olson JL, Schwartz MM, Silva F, eds. Heptinstall's Pathology of the Kidney. Philadelphia: Lippincott-Raven; 1998. p. :1059-95.
- [Google Scholar]
- Clinicopathologic characteristics and outcomes of renal thrombotic microangiopathy in anti-neutrophil cytoplasmic autoantibody-associated glomerulonephritis. Clin J Am Soc Nephrol. 2015;10:750-8.
- [Google Scholar]
- Wegener's granulomatosis presenting as acute suppurative interstitial nephritis. J Clin Pathol. 2001;54:787-9.
- [Google Scholar]
- Changing picture of renal cortical necrosis in acute kidney injury in developing country. World J Nephrol. 2015;4:480-6.
- [Google Scholar]
- Renal cortical necrosis: A life-threatening manifestation of primary antiphospholipid antibody syndrome. Indian J Nephrol. 2016;26:233-5.
- [Google Scholar]






