Translate this page into:
Caught by Surprise - Microfilaria in Renal Biopsies
Corresponding author: Dr. Pallavi Prasad, Room No.-11, C-Block, Department of Pathology, New Diagnostic Block, First Floor, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow - 226 014, Uttar Pradesh, India. E-mail: pallavisgpgi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Prasad P, Gupta N, Verma R, Prasad N, Kaul A, Agrawal V, et al. Caught by Surprise - Microfilaria in Renal Biopsies. Indian J Nephrol. 2024;34:257–60. doi: 10.4103/ijn.ijn_129_23
Abstract
Microfilarial parasites can obstruct the lymphatic tree giving rise to varying lymphatic and extra-lymphatic symptoms. Renal manifestations can range from asymptomatic proteinuria, chyluria, and nephrotic syndrome, to acute glomerulonephritis. The diagnosis of filariasis is usually made by the demonstration of the parasite in the peripheral blood smear, with or without eosinophilia. The renal involvement by this parasite has been sparsely reported in the literature. We hereby report five cases of filariasis detected on histopathological examination of renal biopsies, performed for other indications, along with a brief report of the additional histological findings. Three native and two graft biopsies were included. All our patients were male, with a mean age of 47 years (range 37 to 66 years). The serum creatinine ranged from 1.2 to 12.9 mg/dL. The mean 24-hour urinary protein was 3.6 gm/day. Peripheral blood eosinophilia was not recorded in any case, however, ESR was raised in all cases. Urine examination revealed varying proteinuria, with hematuria in two cases. Histological examination revealed microfilaria in all five biopsies, along with focal segmental glomerulosclerosis in two cases, combined cellular and humoral rejection, minimal change disease and acute tubular necrosis in one case each respectively. All patients were treated with diethylcarbamazine 6mg/kg/day or 12 days, in addition to the renal medications. Diagnosing the parasite is crucial as the patient is likely to benefit due to the timely treatment of the disease. Reporting this case series highlights an interesting finding in nephropathology.
Keywords
Histopathology
microfilaria
proteinuria
renal biopsy
Introduction
Lymphatic filariasis caused by Wuchereria bancrofti and Brugia malayi affects over 120 million people in various tropical and sub-tropical countries. The parasitic infection can obstruct the lymphatic tree, which may either remain asymptomatic or exhibit varying lymphatic and extra-lymphatic symptoms. Renal manifestations range from asymptomatic proteinuria, chyluria, and nephrotic syndrome, to acute glomerulonephritis.1
The diagnosis of filariasis is usually made by the demonstration of a parasite in a peripheral blood smear, with or without eosinophilia. Kidney biopsy is not performed for the diagnosis. Hence, only a few studies have been able to document renal histology in such cases. Only a few case reports document the diagnosis of filariasis made by identifying microfilaria on kidney biopsy.2,3,S1,S2 We report here five cases of filariasis detected on histopathological examination of renal biopsies.
Case Series
Five cases (three native and two transplants) showed the presence of microfilarial parasites on renal biopsy [Figure 1a-f], the prevalence being 0.17%. The key morphological features include a short head space, discrete nuclei in the body, and the column of nuclei does not reach up to the tail tip. The laboratory parameters, indications, clinical diagnosis, and histological findings of renal biopsies are summarized in Table 1. All patients were male, and the mean age was 47 years (range 37–66 years). The serum creatinine ranged from 1.2 to 12.9 mg/dL and the mean 24-hour urinary protein was 3.6 g/day. Peripheral blood microfilaria or eosinophilia was not recorded in any case; however, ESR was raised in all cases. Urine examination revealed varying degrees of proteinuria; however, hematuria was present in two cases only. Thereafter, cases 2, 3, 4, and 5 underwent filarial antigen test, which was positive in all of them. Case 1, however, was lost to follow-up. All patients were treated with anti-filarial agents [diethylcarbamazine (DEC) 6 mg/kg/day for 12 days], in addition to the other prescribed renal medications.
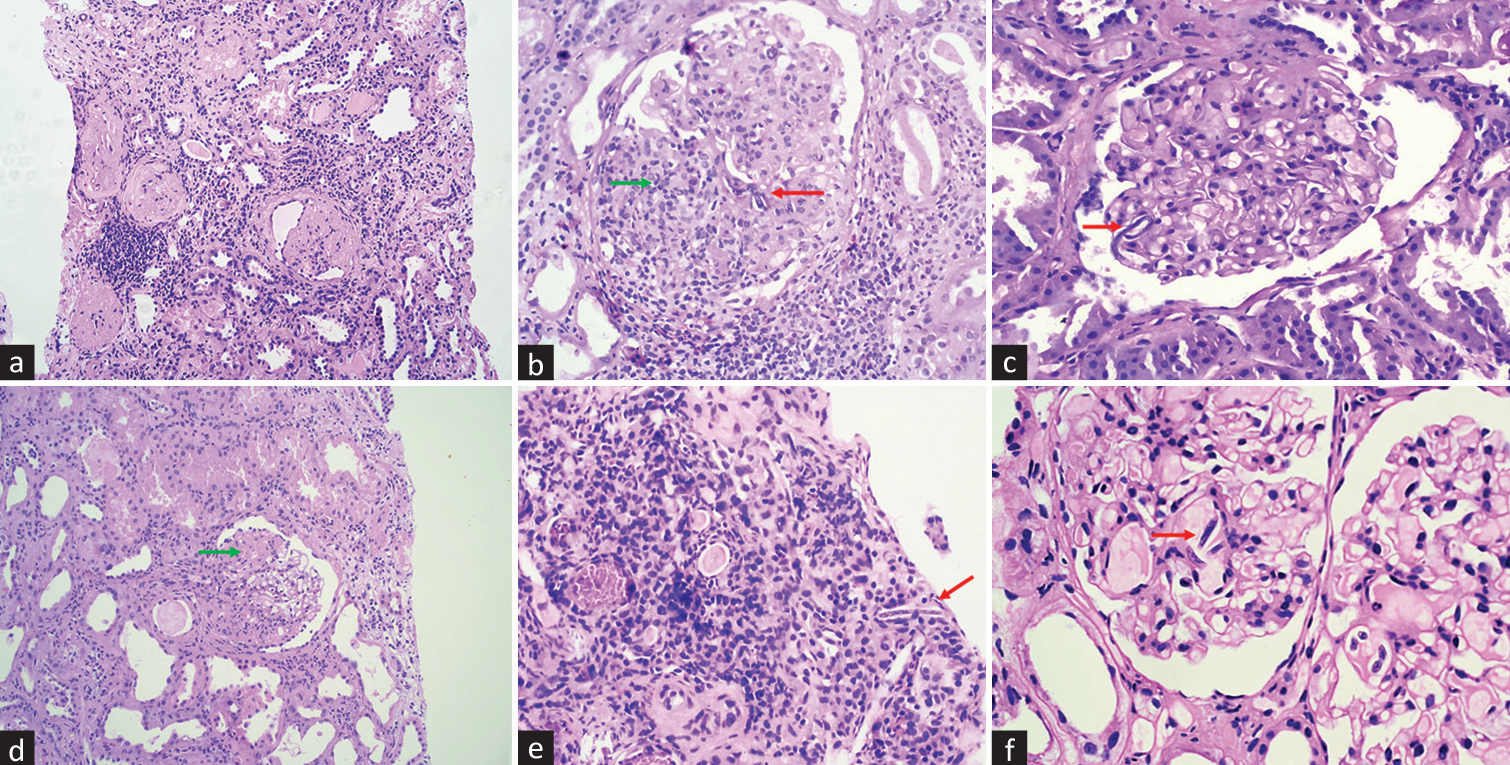
- Case 1: (a) Renal biopsy from the first case showing tubulointerstitial inflammation, suggestive of cellular rejection (H and E × 10). (b) Glomerulitis (green arrow) along with microfilaria in the capillary lumen (red arrow) (H and E × 20). Case 2: (c) Histologically unremarkable glomerulus with microfilaria in capillary lumen (red arrow) (H and E x20). Case 3: (d and e) Glomerulus showing segmental sclerosis (green arrow), with microfilaria in a peritubular capillary (red arrow) (H and E × 40). Case 4: (f) A capillary loop revealing three microfilariae (red arrow) (H and E × 40). This biopsy had a lesion of segmental sclerosis in another glomerulus (H and E × 20). H and E = hematoxylin and eosin.
| Parameters recorded | Case 1 (G) | Case 2 (N) | Case 3 (G) | Case 4 (N) | Case 5 (G) |
|---|---|---|---|---|---|
| Age/gender | 46/M | 66/M | 45/M | 37/M | 41/M |
| Comorbidities, past history | Diabetes mellitus | Nil | Hypertension, tuberculosis (on medication) | Hypertension, anxiety disorder (on medication) | Hypertension, diabetes mellitus, SIADH |
| Hematology | |||||
| Hemoglobin (g/dL) | 7.2 | 13.0 | 10.2 | 13.9 | 6.8 |
| WBC count (×1000/mm3) | 7.6 | 8.3 | 11.5 | 13.1 | 14.1 |
| Eosinophil% | 6% | 2% | 4% | 1% | 3% |
| Platelet count (×106/mm3) | 195 | 402 | 208 | 155 | 253 |
| ESR (mm Hg) | 26 | 32 | 14 | 20 | 22 |
| Chemistry | |||||
| Serum creatinine(mg/dL) | 12.9 | 1.7 | 5.0 | 1.2 | 10.8 |
| 24-hour urinary protein(g/day) | 1.3 | 4.1 | 2.6 | 5.8 | 4.1 |
| Urine | |||||
| pH | 6.5 | 7.5 | 7.0 | 6.0 | 7.0 |
| protein/glucose/red blood cells | 1+/nil/nil | 3+/nil/trace | 2+/nil/trace | 3+/nil/3+ | 3+/nil/1+ |
| Clinicopathological findings | |||||
| Indication of renal biopsy | Advanced renal failure | Mild renal failure, nephrotic range proteinuria, bland sediments | Advanced renal failure | Proteinuria, microscopic hematuria, mild renal dysfunction | Raised serum creatinine |
| Clinical diagnosis | Rejection | MCD, FSGS | Rejection, viral cytopathy | IgA, FSGS | Rejection |
| Primary histological diagnosis | Combined cellular and active antibody mediated rejection | MCD | FSGS with acute pyelonephritis | Focal segmental glomerulosclerosis | Acute tubular necrosis |
| Immunofluorescence | |||||
| IgG, IgM, IgA, C3, C1q | Negative | Negative | IgM, C3 (1 to 2+) | IgM (2+), C3 (3+) | Negative |
| C4d | 70% | - | Negative | - | Negative |
| Electron microscopy | cellular and active antibody mediated rejection | podocytopathy | Transplant glomerulopathy (cg1), multilamination of peritubular capillaries | podocytopathy | Transplant glomerulopathy (cg1) |
G-graft, N-native, MCD-minimal change disease, FSGS-focal segmental glomerulosclerosis, IgA-immunglobulin A nephropathy, SIADH-syndrome of inappropriate secretion of antidiuretic hormone, ESR-erythrocyte sedimentation rate.
Case 1: A kidney transplant recipient, resented with a history of loose stools and a creeping rise of serum creatinine. Light microscopy (LM): Sections included 13 glomeruli, of which five were globally sclerosed and the rest were unremarkable. There was moderate tubular atrophy (ct2), moderate interstitial inflammation (i2), and fibrosis (ci2). Peritubular capillaritis (ptc2) and glomerulitis (g2) were seen. The blood vessels showed medial hyperplasia and focal hyalinosis (ah1). Few glomerular capillary lumens showed the presence of microfilaria. He underwent plasmapheresis, was given DEC, thereafter creatinine reduced, urine output increased to >2 L/day, and was discharged.
Case 2: The patient presented with reduced GFR and nephrotic range proteinuria. LM showed seven unremarkable glomeruli (with microfilaria), tubulointerstitial compartment, and blood vessels. The patient was initiated on steroids and DEC. Creatinine was 1.8 mg/dL on the last follow-up.
Case 3: HIV-positive live-related renal transplantation (2012 presented with complaints of fever, diarrhea, and weight loss four years after transplant. Investigations are shown in Table 1. LM showed ten unremarkable glomeruli. The tubules showed leukocyte casts along with focal acute tubular injury. Interstitium showed dense mixed inflammation including plasma cells and foci of eosinophils. Microfilaria was noted in the peritubular capillaries. Proteinuria was reduced to 1.2 g/day, and creatinine was 2.8 mg/dL on the last follow-up following treatment with steroids and DEC.
Case 4: The patient presented with nephrotic range proteinuria and active urinary sediments. LM revealed 12 glomeruli, one displaying segmental sclerosis and mild tubular atrophy. Few glomerular capillary lumens showed the presence of microfilaria. Proteinuria was 2.7 g/day at the last follow-up, following treatment with steroids, angiotensin-converting enzyme inhibitors, angiotensin-receptor blockers, and DEC.
Case 5: The patient presented with a progressive, rapid rise in serum creatinine. LM included 18 unremarkable glomeruli, however, diffuse acute tubular injury was noted. There were no features suggestive of rejection. Microfilaria was noted in a single glomerular capillary lumen. He was initiated on maintenance hemodialysis and DEC.
Discussion
Lymphatic filariasis is a tropical disease transmitted by different mosquito species: Culex, Anopheles, Mansonia, and Aedes. It has varied clinical presentations where some patients may be asymptomatic, while others may harbor acute disease which may progress to chronic debilitating symptoms. Filariasis classically manifests as peripheral blood eosinophilia, lymphangitis, and lymphoedema. The commonest species implicated in the Indian subcontinent is Wuchereria bancrofti, followed by Brugia malayi.4
Renal involvement is known to be caused by infection with both organisms.S3 Renal abnormalities may be caused by (a) mechanical damage to the glomeruli and (b) deposition of immune complexes. The glomerular disease associated with filariasis is predominantly immune-complex-mediated and diffuse mesangial hyperplasia is the most common histology.S4 Membranous nephropathy has also been described in the literature.S5 Nayak et al.5 reported a case of AA-type renal amyloidosis in a patient with chronic filariasis. However, the parasite was not found in the biopsy but was identified in the blood only. Clinical presentation of chyluria and rare instances of finding microfilaria in the renal biopsy specimen has also been described. Three of our cases presented with nephrotic range proteinuria. It is difficult to ascertain if the filarial parasite in these cases was also contributing to proteinuria, or was the sole effect of the respective renal lesions, i.e. minimal change disease (MCD) and focal segmental glomerulosclerosis (FSGS). Hence, it may be difficult to conclude that the presence of filarial parasites was merely an incidental finding. In the fifth case, however, the finding of early transplant glomerulopathy accounted for proteinuria.
The microfilaria in circulation leads to mechanical damage of glomeruli, thereby causing hematuria, as seen in 2 of our cases.S6 Microfilarial antigens are increased in circulation, which can correlate with adult worms’ heightened metabolic activity. This leads to the formation and deposition of immune complexes in the glomerular basement membrane as well as direct mechanical damage to the tubulointerstitium. Dreyer et al.6 stated that DEC therapy leads to the disintegration of dead microfilaria, causing the deposition of immune complexes, which in turn may lead to proteinuria and hematuria.
The conventional method of diagnosis by demonstration of microfilariae in peripheral blood smear has a low sensitivity (3–6%). Serological tests having very high sensitivity and specificity include enzyme-linked immunosorbent assay (ELISA) and rapid immunochromatographic card test for circulating antigens of Wucheraria bancrofti.S7 DEC 6 mg/kg for 12 days is recommended as the standard monotherapy.
Conclusion
It is uncommon to encounter filarial parasite in renal biopsy specimens. Our patients presented with variable degrees of proteinuria with or without hematuria. Diagnosing the parasite is crucial as the patient is likely to benefit due to the timely treatment of the disease. Reporting of this case series is an addition to a rare, yet interesting finding in nephropathology.
Conflicts of interest
There are no conflicts of interest.
References
- Microfilaria in kidney biopsy: A report of two cases. J Infect Public Health. 2018;11:732-4.
- [CrossRef] [PubMed] [Google Scholar]
- Amyloidosis kidney with filariasis presenting as nephrotic syndrome: Incidental finding or unusual association? Trop Med Health. 2008;36:185-7.
- [CrossRef] [Google Scholar]
- Secondary collapsing glomerulopathy associated with Loa loa filariasis. Am J Kidney Dis. 1997;30:836-9.
- [CrossRef] [PubMed] [Google Scholar]
- Filariasis presenting with bicytopenia, progressive splenomegaly and acute renal failure: An unusual case report. Trop Doct. 2021;51:588-90.
- [CrossRef] [PubMed] [Google Scholar]
- A rare case of reversible acquired AA-type renal amyloidosis in a chronic filariasis patient receiving antifilarial therapy. Clin Exp Nephrol. 2011;15:591-5.
- [CrossRef] [PubMed] [Google Scholar]
- Extralymphatic disease due to bancroftian filariasis. Braz J Med Biol Res. 1999;32:1467-72.
- [CrossRef] [PubMed] [Google Scholar]







