Translate this page into:
Comparison of vascular access use in hemodialysis patients in Isfahan in 2003 and 2013
Address for correspondence: Dr. Maryam Soheilipour, Department of Internal Medicine, Isfahan University of Medical Sciences, Isfahan, Iran. E-mail: m_soheilip@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Vascular access (VA) complications are the leading cause of morbidity in the hemodialysis (HD) population and responsible for high health care costs. This study was designed to compare the profile of VA use for HD in Isfahan dialysis units in 2003 and 2013. A cross-sectional observational study was conducted between January and March 2013 on 536 HD patients in seven units. The patients data about VA type, number, survival, and demographic characteristics were collected and compared with the data collected in year 2003 on 320 patients in the same city units. The mean age of patients increased from 51 ± 17 to 58 ± 15 years (P < 0.001). The most common etiology of end-stage renal disease was diabetes mellitus, but the percentage increased in 2013 (P = 0.001).The use of an arteriovenous fistula (AVF) as a first dialysis access fell from 60.6% in 2003 to 35.4% in 2013 (P < 0.001). At the time of study, AVFs were used in 92.2% of patients in 2003 versus 56.5% in 2013 (P < 0.001). The 1, 2, 3 and 5 years AVF survival was 80%, 78%, 73%, and 69%, respectively in 2003 versus 79.4%, 61.2%, 47.3%, and 31.5% in 2013. The AVFs proportions decreased and the tunneled catheters proportions increased while the proportion of temporary catheters decreased in 2013 compared with 2003.
Keywords
Arteriovenous fistulae
catheter
hemodialysis
vascular access
Introduction
The population of patients with end-stage renal disease (ESRD) is on a progressive growth worldwide. Hemodialysis (HD) is the major mode of renal replacement therapy.[1] A well-functioning vascular access (VA) is an important aspect of efficient dialysis therapy. VA complications remain the leading cause of morbidity in the HD population and responsible for high health care costs[2345] and provides quantity and quality of life to the ESRD patients.[6]
There are three main types of permanent access: native arteriovenous fistulas (AVFs), AV graft (AVG) and tunneled catheters (TCs). Non-tunneled central vein catheters (CVCs) are used as temporary access.[27] Catheter use is associated with higher rates of infection and could compromise dialysis adequacy.[8910] AVF is the optimal vascular access because of superior patency rates, with fewer interventions, lower infectious complications, and improved performance over time.[11121314] Guidelines from different countries strongly recommend AVF use.[15]
The National Kidney Foundation's Dialysis Outcomes and Quality Initiative (NKF KDOQI) guidelines recommend that patients with advanced chronic kidney disease, (glomerular filtration rate <30 mL/min/1.73 m2) should be evaluated for AVF creation, while HD is proposed as the renal replacement therapy modality of choice. These guidelines also recommend that AVF be placed in 50% of all incident and 40% of all prevalent dialysis patients.[16]
In new dialysis patients, early referral to a nephrologist and early patient training predict a successful permanent VA function at dialysis initiation. AVF survival is also better when used for the first HD treatment.[1217] Despite intensive efforts in reducing the use of catheters; the data from the Forum of ESRD Networks suggest that 21% of prevalent HD patients are dialyzed with a CVC for ≥90 days. This certainly exceeds the NKF-KDOQI published recommendations of <10% CVC prevalence.[18]
This study was designed to compare the profile of VA use for HD in Isfahan dialysis units in year 2003 and 2013.
Materials and Methods
This is a cross-sectional observational study conducted from January to March 2013, in seven HD units (Alzhra, Noor, Shariati, Sadooghi, Amin, Hojjatiye and Zahraye Marziye). A total of 536 prevalent HD patients were evaluated.
Each HD unit was visited by the researchers and data were collected through questionnaires by interviewing patients, physical examination and reviewing patient records. An informed consent was obtained from all patients. The patients of both genders aged over 16-year-old who were on HD at least for 1 month and were in agreement with the consent term included. The mentioned procedures were in accordance with the ethical standards of the committee on human experimentation of Isfahan Medical University.
Following variables were evaluated: Sex, age, duration of HD, underlying disease, time between the creation of the first AVF and the beginning of HD; data regarding VA utilization including: Type, number, placement location and survival of actual and previous accesses; history of kidney transplant and its duration; history of glucocorticoid consumption.
The results were compared with the data collected through the study performed in 2003 on 320 patients aged over 16-year-old who were on HD at least for 1 month in all dialysis units of our city. In mentioned study, researchers evaluated demographic variables, duration of HD, underlying disease, and data regarding VA utilization.[19]
Data analysis
The variables are presented as means ± standard deviation and percentages. Analysis was performed using SPSS version 20 statistical software (IBM company). P < 0.05 was considered to be statistically significant. Survival of AVF was assessed through Kaplan-Meier survival curve. Independent t-test and Chi-square test were applied for comparing the variables here with the previous study.
Results
Patient characteristics during two study periods are listed in Table 1. The mean age of patients increased from 51 ± 17 (range 16-88) to 58 ± 15 (range 18-91) years (P < 0.001). The duration of HD in 2003 and 2013 was 28 ± 31 (range 1-168) and 37 ± 38 (range 1-240) months (P < 0.001). The most common etiology of ESRD was DM in both years, but the percentage significantly increased in 2013 (P = 0.001). There was no significant change in gender distribution (P = 0.52).

The use of an AVF as a first dialysis access fell from 60.6% in 2003 to 35.4% in 2013 (P < 0.001). Figure 1 shows a comparison of VA use at the start of HD between two study periods. At the time of study, AVFs were used in 56.5% of patients in 2013 versus 92.2% in 2003 (P < 0.001) [Figure 2].

- Comparison of vascular access type at the start of hemodialysis in year 2003 and 2013. AVG: Arteriovenous graft, AVF: Arteriovenous fistula
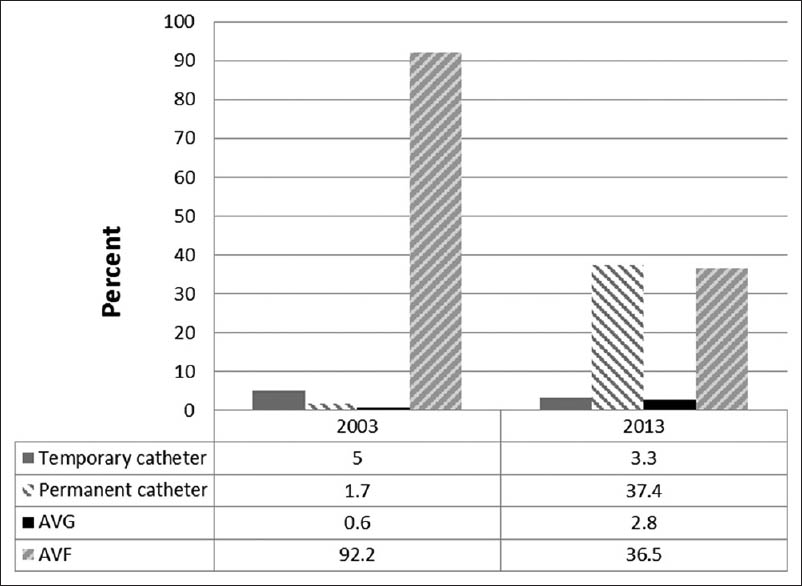
- Comparison of vascular access type at the time of study in year 2003 and 2013. AVG: Arteriovenous graft, AVF: Arteriovenous fistula
Of the total number of 951 permanent VA used in 2013 group, 47.7% were AVFs, 3.3% AVGs and 49% were TCs. Among 210 temporary catheters 164 (78%) were placed in the jugular vein and 46 (22%) in the femoral vein; whereas in 2003, from the total number of 412 permanent VA, 97.3% were AVFs, 1% AVGs and 1.7% were TCs and among 207 temporary catheter used during dialysis 145 (70%) were placed in jugular vein, 39 (18.8%) in the femoral vein and 23 (11.2%) in subclavian vein.
In 2003, 53.1% of AVFs were placed in wrist (radiocephalic), whereas in 2013 only 9.5% of AVFs placed in the wrist and the entire was in elbow (brachiocephalic).
The 1, 2, 3 and 5 years AVF survival were 79.4%, 61.2%, 47.3%, and 31.5%, respectively, in 2013 [Figure 3] versus 80%, 78%, 73%, and 69% in 2003. Primary failure of AVF was 8.2% in 2013 versus 13% in 2003.

- Arteriovenous fistula survival by Kaplan–Meier in 2013
The graft use increased slightly from 2003 to 2013 at a constant low level (0.6% vs. 2.8% [P = 0.03]).
The maximum number of accesses that each patient used during dialysis was seven in 2013. The number of accesses used by each patient in two studies is shown in Table 2.

The following results were obtained from the study population in 2013. These variable were not evaluated in 2003.
Before the start of HD therapy 212 (39.5%) patients had AV fistula. The mean duration from placing an AV fistula until starting HD was 11 ± 24 months (minimum 1 and maximum 144 months). Among these patients, 190 (35.4%) used an AV fistula as their first AV access. Among the created fistula for dialysis patients, 97% of them were placed by a vascular surgeon and mean duration of use was 40 ± 44 months. A total of 110 patients (20.6%) had no fistula or graft.
The mean use duration of temporary catheter was 42 ± 18 days for jugular CVC (minimum of 1 week up to 4 months) and 11 ± 6 days (minimum of 1 week up to 1 month) for femoral CVC. The mean use duration of permanent catheter was 11 ± 8 months (minimum of 2 weeks up to 42 months).
Forty-seven patients underwent kidney transplantation, with a mean graft survival of 74 ± 51 (range 0 -192) months.
Discussion
The periodic review of access for HD needs to be performed by all dialysis units in order to monitor their adequacy in observation of the international guidelines. Accordingly, an investigation was performed in HD units to analyze the changes observed in the profile of the VA used in 2013 compared to that in 2003 in the same dialysis units.
The main finding of this study indicates a significant decrease in the proportion of AVFs and an increase in the proportion of TCs in 2013 compared with 2003 for the beginning and duration of HD. Until 2003, the use of AVFs was above the targets recommended by KDOQI guidelines. However, its use declined at the expense of increasing use of TCs.[16]
By contrast, a decrease in temporary catheter use at the initiation of HD was observed. This decrease in temporary catheter use is due to a greater trend in TC use as a bridging catheter. These results are similar to those reported by Malek et al.[20] in a dialysis unit in Spain that no incident patient had a TC inserted in 2000, while 23.7% had TCs in 2005; and also they observed a decreased use of temporal catheters (from 16.6% to 7%) in their patients.
In a study in North America in 2007, the frequency of VA was studied on 25,003 incident dialysis patients: 19,622 (78.5%) initiated dialysis with a catheter; 4151 (16.6%), with a fistula; and 1230 (4.9%), with a graft. At 90 days, 14,105 (69.7%) had a catheter, 4432 (21.9%) had a fistula, and 1705 (8.4%) had a graft.[21]
From 1996-2007, use of AVF rose from 24% to 47%, use of graft fell from 58% to 28% and use of catheter increased from 17% to 25% in USA (TCs comprise 80-95% of used catheters). A trend toward greater TC use was also observed in other countries between Dialysis Outcomes and Practice Patterns Study-I and III.[3]
In our study, the most frequent AVF location changed from wrist (radiocephalic) to elbow (brachiocephalic). This change in VA location does not correspond to the guidelines that recommend placing a wrist (radio cephalic) AVF as a first option.[7] The 1 year AVF survival is similar in both the studies (2003 and 2013), while the 2, 3 and 5 year survival decreased significantly in 2013 (P < 0.001). In one study, the estimated 1-year survival for AVF was 68% in US and 83% in Europe.[2] In other study, the primary and secondary patency rates were 52% and 62% at 5 years for brachiobasilic and 40% and 46% at 5 years for brachiocephalic fistula, respectively.[22] In Nigerian, 1-year AVF survival was 63.2%.[23]
The use of TCs has begun from 2003 in our city and its survival rose from 6.1 ± 0.8 to 10.9 ± 8.25 months from 2003-2013.[24]
The KDOQI guidelines specify early referral to a nephrologist and determination of the patient's preferred dialysis modality as the best means of increasing the percentage of AV fistulae.[17] Some reports focus on the role of additional measures that minimize the TC use, such as peritoneal dialysis, VA education, pre-operative vascular mapping and the rescue of early failure and thrombosed fistula.[25] For patients are not fit for AVF creation, a graft might be a better option.
Results of different studies suggest that the use of TC is associated with greater risk of sepsis, hospitalization and mortality and it is the last choice after the AV F and AVG.[7] Considering these facts, the high level of catheter use in our dialysis units is a matter of concern and it should lead to an immediate action.
A limitation of this study is its retrospective nature and lack of information to explain the exact reasons of this change in VA profile during this decade. Moreover, the results of this study only reflect the trend of VA use in Isfahan city and no data is available to compare this trend to other centers.
Future prospective studies should be conducted to analyze the potential influence of different factors on this change. Team works should focus on training all involved people in predialysis care, including the patients, referring physicians, surgeons, and nephrologists.
Conclusions
The results of this study revealed a significant decrease in the proportions of AVFs and also an increase in the percentage of the patients with the TCs. While the proportion of temporary catheters decreased in 2013 compared with that of in 2003 for the beginning and duration of HD, the graft use has still remained at a low level.
Acknowledgment
This work was supported by Isfahan University of Medical Sciences (Project number: 392016).
Source of Support: This work was supported by Isfahan University of Medical Sciences. (Project number: 392016)
Conflict of Interest: None declared.
References
- Vascular mapping: Does it help to maximize fistulae placement? Adv Chronic Kidney Dis. 2009;16:316-20.
- [Google Scholar]
- Vascular access use in Europe and the United States: Results from the DOPPS. Kidney Int. 2002;61:305-16.
- [Google Scholar]
- Vascular access use and outcomes: An international perspective from the dialysis outcomes and practice patterns study. Nephrol Dial Transplant. 2008;23:3219-26.
- [Google Scholar]
- An experience of vascular access for hemodialysis in Brazil. Int Arch Med. 2011;4:16.
- [Google Scholar]
- Epidemiology of vascular access for hemodialysis and related practice patterns. Contrib Nephrol. 2004;142:14-28.
- [Google Scholar]
- The endless history of vascular access: A surgeon's perspective. J Vasc Access. 2006;7:103-11.
- [Google Scholar]
- Access for starting kidney replacement therapy: Vascular and peritoneal temporal access in pre-dialysis. Nefrologia. 2008;28(Suppl 3):105-12.
- [Google Scholar]
- Fourteen years of hemodialysis with a central venous catheter: Mechanical long-term complications. J Vasc Access. 2006;7:60-5.
- [Google Scholar]
- Effects of starting hemodialysis with an arteriovenous fistula or central venous catheter compared with peritoneal dialysis: A retrospective cohort study. BMC Nephrol. 2012;13:88.
- [Google Scholar]
- Vascular access morbidity and mortality: Trends of the last decade. Clin J Am Soc Nephrol. 2013;8:1213-9.
- [Google Scholar]
- Complications of arteriovenous fistulae: Beyond venous stenosis. Adv Chronic Kidney Dis. 2012;19:195-201.
- [Google Scholar]
- Hemodialysis vascular access modifies the association between dialysis modality and survival. J Am Soc Nephrol. 2011;22:1113-21.
- [Google Scholar]
- Duration of temporary catheter use for hemodialysis: An observational, prospective evaluation of renal units in Brazil. BMC Nephrol. 2011;12:63.
- [Google Scholar]
- Retrospective analysis of 271 arteriovenous fistulas as vascular access for hemodialysis. Indian J Nephrol. 2013;23:191-5.
- [Google Scholar]
- Vascular access in patients receiving hemodialysis in Libya. J Vasc Access. 2012;13:468-74.
- [Google Scholar]
- NKF-KDOQI. Clinical practice guidelines for vascular access: Update 2006. Am J Kidney Dis. 2006;48:248-72.
- [Google Scholar]
- Timing of nephrologist referral and arteriovenous access use: The CHOICE Study. Am J Kidney Dis. 2001;38:494-501.
- [Google Scholar]
- Complications of catheters: Tunneled and nontunneled. Adv Chronic Kidney Dis. 2012;19:188-94.
- [Google Scholar]
- Prevalence of vascular access, survival in patients with end stage renal disease. Tehran Univ Med J (TUMJ). 2005;62:960-6.
- [Google Scholar]
- Changes in vascular access in a dialysis unit in recent years: Planning problems, change in preferences, or demographic change.? Nefrologia. 2008;28:531-8.
- [Google Scholar]
- Hemodialysis access usage patterns in the incident dialysis year and associated catheter-related complications. Am J Kidney Dis. 2013;61:123-30.
- [Google Scholar]
- Evaluation of the efficacy of the transposed upper arm arteriovenous fistula: A single institutional review of 190 basilic and cephalic vein transposition procedures. J Vasc Surg. 2007;46:94-99.
- [Google Scholar]
- Outcome and complications of permanent hemodialysis vascular access in Nigerians: A single centre experience. Ann Afr Med. 2013;12:127-30.
- [Google Scholar]
- Studying the survival of permanent catheters for hemodialysis in Isfahan. MSD Thesis. Isfahan University of Medical Sciences 2005
- [Google Scholar]
- Strategies to minimize tunneled hemodialysis catheter use. Blood Purif. 2006;24:90-4.
- [Google Scholar]







