Translate this page into:
Congenital Unilateral Hypoplasia of Kidney with Mesonephric Remnants in the Ureter: A Case Report
Address for correspondence: Dr. Mukta Pujani, Department of Pathology, ESIC Medical College, Faridabad, Haryana, India. E-mail: drmuktapujani@gmail.com
-
Received: ,
Accepted: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Mesonephric remnants persist as an appendix of epididymis and paradidymis in efferent ductules in males and skene’s glands and Gartner’s ducts in females. The mesonephric remnant in the renal parenchyma is extremely rare and only a few cases have been reported in the literature. We present a case with a non-functioning atrophic left kidney. Histopathology showed variable-sized ducts filled with colloid-like material surrounded by collagenized stroma. The ureter showed hypertrophied muscle and a few ducts lined by flattened and a few by columnar epithelium resembling epididymis suggestive of mesonephric remnants. IHC for CD10, PAX 8, and GATA3 was positive. A diagnosis of congenital unilateral hypoplasia of kidneys and ureter with mesonephric remnants was given.
Keywords
GATA 3
hypoplastic kidney
mesonephric remnants
Introduction
Renal anomalies such as renal agenesis and multicystic dysplastic kidney (MCDK) are usually associated with the absence of a ureter or an atretic one. Rarely, these renal anomalies may also be associated with the dilated tortuous ureter, ureterocele, or other cystic malformation of mesonephric duct (MND) remnants.[1] Mesonephric ducts are embryonic structures, which drain from the mesonephric kidney to the urogenital sinus. The influence of testosterone from the testes in the males’ results in the formation of the epididymis, ductus deferens, and ejaculatory duct derived from portions of the mesonephric duct. In females, however, it regresses completely during the developmental process.[2] Mesonephric remnants persist as an appendix of epididymis and paradidymis in efferent ductules in males and skene’s glands and Gartner’s ducts in females.[3] The rare locations of mesonephric remnants in the males include the renal pelvis, spermatic cord, vas deferens, urethra, and prostate.[3] The mesonephric remnants may proliferate and may become hyperplastic and also occasionally may result in malignant transformation, leading to mesonephric carcinoma.[4] Although cases of mesonephric remnants (MR) are reported in the pelvis including the genitourinary tract in both the males and females, only a few cases of mesonephric remnants have been reported in the renal parenchyma[3456] in the literature.
Hence, we report a case of a unilateral nonfunctional hypoplastic kidney with the presence of mesonephric remnants in the kidneys and ipsilateral ureter, which is extremely rare.
Case Report
A 29-year-old male presented with the chief complaint of left flank pain on and off for 2 years. Ultrasonography and computed tomography revealed a atrophic left kidney [Figure 1]. The renal DTPA (diethylenetriaminepentacetate) scan result no function on left side. The other kidney was normal in structure and function. No other anomalies were detected.
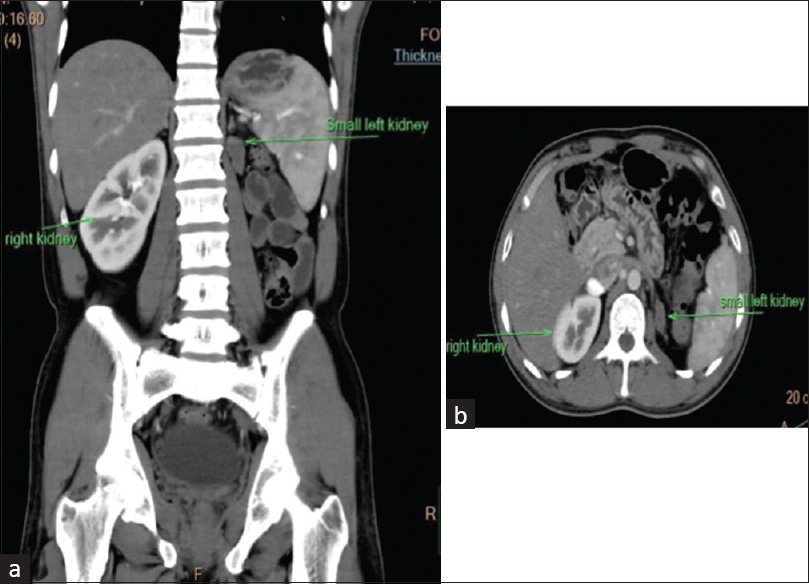
- Computed tomography images show a markedly atrophic left kidney. (a: Longitudinal plane and b: Transverse plane)
Modified radical nephrectomy was done and the specimen was sent for histopathology. The gross specimen consisted of a markedly atrophic kidney with attached perinephric fat. The ureter could not be accurately identified grossly; however, a small tubular structure was processed as ureter. On the cut section, no corticomedullary distinction was possible in the renal parenchyma. Microscopy revealed many dilated structures, some of them lined by tall columnar ciliated cells with an underlying layer of low cuboidal cells. Also, many variable-sized ducts were arranged in a vague lobular pattern filled with colloid-like material, a few of them showing calcification and were surrounded by collagenized stroma along with small-to-medium-sized blood vessels [Figure 2]. There was an absence of stromal proliferation, and no heterologous elements or blastemal component was identified. Thus, renal mesenchymal neoplasms and Wilms’ tumor were excluded. The section from the ureter showed hypertrophied muscles and a few ducts lined by flattened or columnar epithelium resembling epididymis suggestive of mesonephric remnants [Figure 2 inset]. Immunohistochemistry (IHC) for CD10 and GATA3 was positive in the epithelia of epididymis type tubules and PAX8 was positive in the epithelia of tubules with a single layer of cuboidal cells [Figure 3]. None of these markers were positive in the stroma. Therefore, based on histopathological findings along with immunohistochemistry, a diagnosis of congenital unilateral hypoplasia of kidneys and ureter showing mesonephric remnants was given.
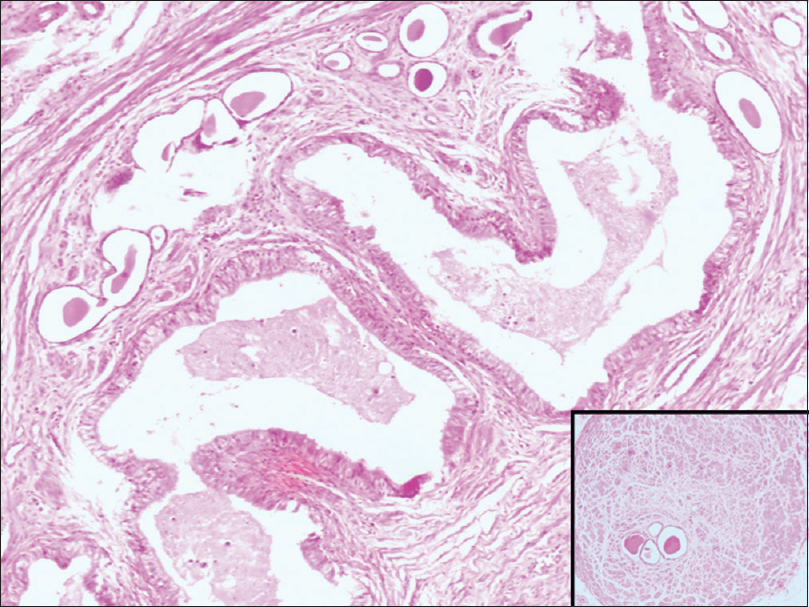
- Section shows dilated tubular structures with tall columnar cells with cilia resembling epididymis and lobules of tubular structures lined by a single layer of cells filled with colloid material. (H&E 100×) Inset showing sections from the ureter with muscular hypertrophy and tubular structures. (H&E 40×)
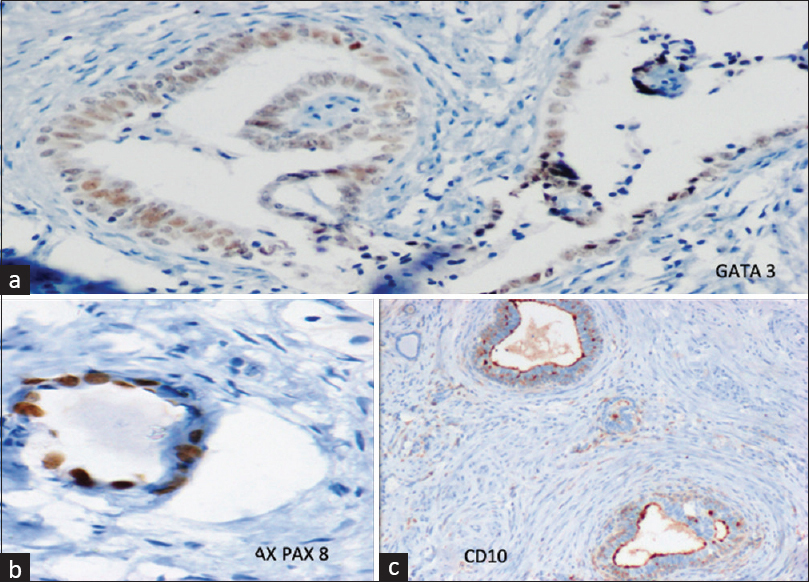
- (a) IHC for GATA 3 showing nuclear positivity in the epithelia of epididymis-like tubular structures. (b) IHC for PAX8 shows nuclear positivity in the epithelia of a tubular structure. (c) IHC for CD10 showing luminal positivity in the epithelia of an epididymis-like tubular structure
Discussion
The mesonephric duct (MND) develops during early gestation and gives rise to the ureter and trigone of the bladder. Around the 28th day, the ureteric bud from the MND contacts the metanephric blastema, and reciprocal activation between these leads to the formation of the kidneys and ureter. The ureter, renal pelvis, calyces, and collecting ducts arise from the ureteric bud, whereas metanephric blastema forms the renal parenchyma. MND forms the vas and epididymis cranially and caudally it is transformed into the ejaculatory duct and a subsequent bud leads to the formation of seminal vesicles.[1] Nephrogenesis requires perfect coordination of all events and also the failure of regression of primary structure may hamper the development of secondary ones and may also lead to the persistence of remnants.[4] MRs have been reported in the urogenital organs of both males and females. In males, it includes the urethra, prostate, renal pelvis, spermatic cord, and vas deferens, and in females, MRs are seen in the cervix, vagina, adnexa, and uterine corpus.[4] Usually, the organs with the mesonephric remnants are well developed and functional; however, occasionally they may be associated with other developmental anomalies such as renal hypoplasia.[4] The MND tubulocystic structures along with renal agenesis or MCDK arise from the ureteric bud structures and present as a ureterocele with or without a blind-ending ureter-like structure.[1] In the present case, the patient presented with a hypoplastic kidney along with a small blind ending ureter-like structure grossly.
The classic mesonephric hyperplasia shows small tubules lined by a single layer of cells with round to oval nuclei with occasional prominent nucleoli. The epididymal type mesonephric hyperplasia showed a tubular structure lined by columnar cells with pseudostratified elongated hyperchromatic nuclei.[2] In the present case, a combination of both classical and epididymal types of mesonephric remnants was noted. This is extremely rare and only one study has been reported in the literature by Xiao et al.,[3] who have reported similar histological findings in the renal parenchyma. Wang et al.[4] also reported mesonephric remnants in the renal parenchyma that resembled epididymis, vas deferens, and seminal vesicles.
The Pax 8 marker is used to demonstrate Mullerian differentiation and stains MR in the prostate and cervix. MRs are also positive for the biomarkers CD10 (showing luminal staining pattern) and calretinin. Howit et al.[7] reported GATA 3 to be a sensitive and specific marker for mesonephric remnants in the female genital tract. There is a paucity of literature on the immunohistochemical staining pattern of the mesonephric remnants in the renal parenchyma. The current case demonstrates positive nuclear staining for CD10, PAX 8, and GATA 3 in the cells lining the epididymis tubules, which is in accordance with a study by Xiao et al.[3] and Wang et al.,[4] thus the mesonephric differentiation was established.
The abnormal embryonic development may lead to various congenital anomalies of the kidneys, which could be due to renal parenchymal malformations, abnormalities in renal migration, or abnormalities in the developing collecting system. The abnormal maturation of the kidneys may lead to congenital urinary anomalies such as renal dysplasia and hypoplasia which are common malformations.[8]
Several signaling pathways are implicated in the pathogenesis of renal hypoplasia, which include GDNF/Ret, fibroblast growth factor, PAX2, and Hedgehog pathways. The nephron number in the kidneys is also affected by several factors affecting the in utero environment; however, the mechanisms are unknown.[9]
MRs have the potential to transform into malignancy[4] and thus intrarenal MR needs to be differentiated from neoplastic lesions such as a metanephric stromal tumor, and metanephric adenofibroma, congenital mesoblastic nephroma (CMN), Wilms’ tumor and renal dysplasia.[34] Metanephric stromal tumor (MST) is an unencapsulated spindle-to-stellate lesion entrapping the native kidney along with onion skin cuffing around the tubules and blood vessels. Heterologous differentiation can also be seen. Similar findings can be seen in CMN; however, it has deeply infiltrative borders.[10] lies between metanephric stromal tumor, which consists of a mainly stromal component, and metanephric adenoma, which is a purely epithelial tumor.[11] The current case did not show any stromal proliferation and consisted of tubular structures lined by cuboidal cells and also tall columnar epithelium with cilia resembling epididymis. The diagnosis of Wilms’ tumor requires the presence triad of mesenchymal, epithelial, and blastemal elements,[12] which was not present in the present case. Renal dysplasia contains disorganized renal tissue containing undifferentiated epithelium, primitive ducts, and fibromuscular connective tissue. The histological features coupled with immunohistochemistry positive for GATA 3 and CD10 in epididymis-like structures and PAX8 in the tubular structures lined by a single layer of cells proved them to be mesonephric rests. Rare cases of MR malignancies have also been reported by authors in sites such as the vagina[13] and the prostate.[14] However, in the present case, there was no mass lesion and histologically no nuclear atypia, necrosis, angiolymphatic invasion, or infiltrative growth was seen, pointing toward a benign process.
Conclusion
The mesonephric rests in the kidneys need to be differentiated from renal mesenchymal tumors and Wilms’ tumor. Although the finding of mesonephric remnants is incidental, the knowledge about this entity is essential as there is a risk of malignancy. The histological features along with immunohistochemistry is essential in arriving at a correct diagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Tubulocystic anomalies of the mesonephric duct associated with ipsilateral renal dysgenesis. J Pediatr Urol. 2019;15:46.e1-6.
- [Google Scholar]
- Hyperplasia of mesonephric remnant, epididymal type: A case report. Basic Appl Pathol. 2009;2:69-71.
- [Google Scholar]
- Unilateral hypoplastic kidney and ureter associated withdiverse mesonephric remnant hyperplasia. Am J Clin Exp Urol. 2015;3:107-11.
- [Google Scholar]
- Hypoplastic kidney with hyperplastic mesonephric remnants as a cause of unilateral non-functioning kidney in an adult male. Hum Pathol Case Rep. 2019;18:200335. doi:10.1016/j.ehpc.2019.200335
- [Google Scholar]
- Epididymis-like tubules in adult renal hypodysplasia: Immunohistochemical features indicate a mesonephric origin. Int J Surg Pathol. 2017;25:206-15.
- [Google Scholar]
- Mesonephric elements in the kidney –Matters of embryology and etymology. Hum Pathol Case Rep 202;20.200364 doi:10.1016/j.ehpc.2020.200364
- [Google Scholar]
- GATA3 is a sensitive and specific marker of benign and malignant mesonephric lesions in the lower female genital tract. Am J Surg Pathol. 2015;39:1411-9.
- [Google Scholar]
- Natural course of children with dysplastic and hypoplastic kidney. World J Nephrol Urol. 2013;2:55-9.
- [Google Scholar]
- Genetics of renal hypoplasia: Insights into the mechanisms controlling nephron endowment. Pediatr Res. 2010;68:91-8.
- [Google Scholar]
- Metanephric stromal tumor: A novel pediatric renal neoplasm. Indian J Pathol Microbiol. 2009;52:389-91.
- [Google Scholar]
- Extrarenal Wilms' Tumor: Challenges in diagnosis, embryology, treatment and prognosis. In: van den Heuvel-Eibrink MM, ed. Wilms Tumor. Brisbane (AU): Codon Publications; 2016. Chapter 6
- [Google Scholar]
- A case of mesonephric adenocarcinoma of the vagina with a 1-year follow-up. Int J Gynecol Cancer. 2008;18:1127-31.
- [Google Scholar]
- Mesonephric remnant hyperplasia involving prostate and periprostatic tissue: Findings at radical prostatectomy. Am J Surg Pathol. 2011;35:1054-61.
- [Google Scholar]







