Translate this page into:
Extensive Tumoral Calcinosis and Acral Osteolysis
Corresponding author: Mohamed Hassanein, Division of Nephrology and Hypertension, University of Mississippi Medical Center, Jackson, United States. E-mail: mhassanein@umc.edu
-
Received: ,
Accepted: ,
How to cite this article: Sriperumbuduri S, Atari M, Hassanein M. Extensive Tumoral Calcinosis and Acral Osteolysis. Indian J Nephrol. 2025;35:307-8. doi: 10.25259/IJN_512_2024
A 39-year-old male on hemodialysis developed painful swelling at the tips of the right index and middle fingers, left elbow and wrist, and right shoulder. X-rays showed calcified densities (blue arrows) in the right index and middle fingers [Figure 1a and b], left wrist [Figure 1c], bilateral shoulders [Figure 1d and e], left elbow [Figure 1f], and left femur [Figure 1g]. Acral osteolysis affected the distal phalanx of right thumb [Figure 1a], right long finger [Figure 1b], and left index finger [Figure 1c]. Labs showed normal serum calcium, elevated phosphate, and elevated parathyroid hormone (PTH) of 1762 pg/mL. Nuclear parathyroid scan revealed hyperplasia of three parathyroid glands. Patient was started on cinacalcet with improvement in PTH level and was referred to endocrine and orthopedic surgery. This case depicts the effects of severe tertiary hyperparathyroidism on the bone resulting in acral osteolysis and tumoral calcinosis.
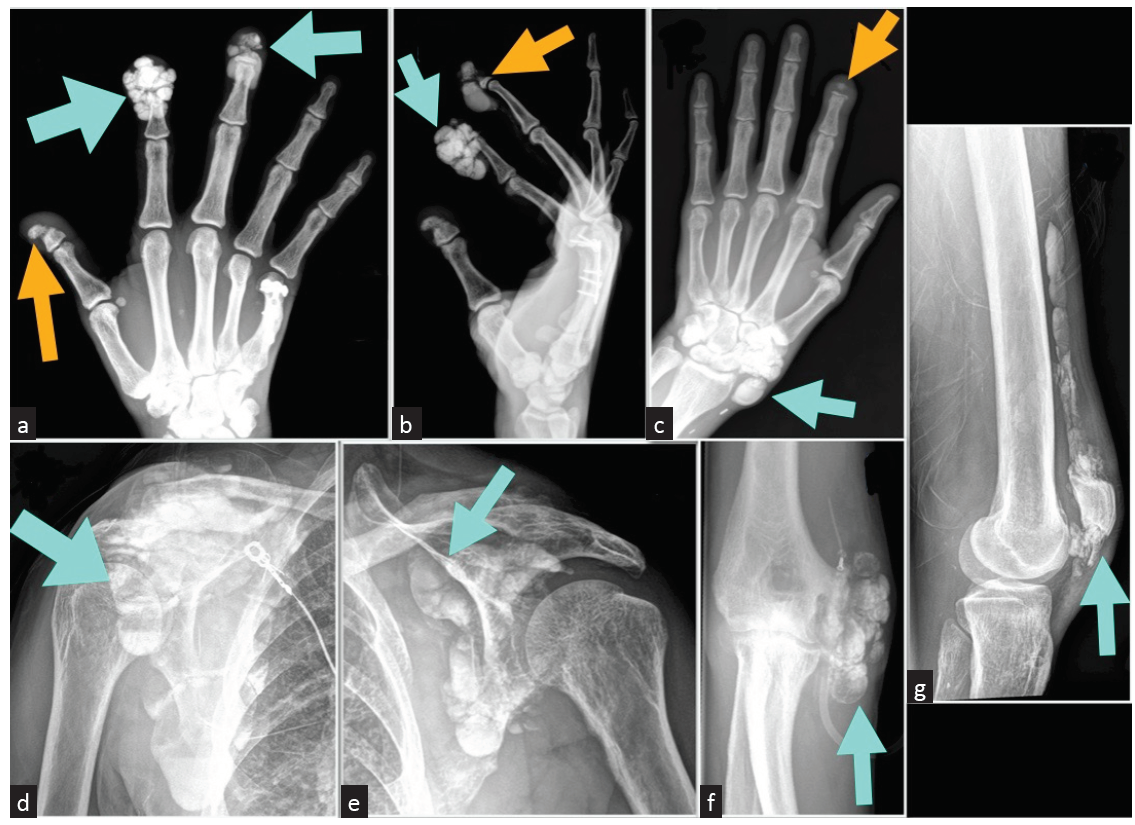
- Plain radiograph showing calcified densities (blue arrows) in the (a and b) right index and middle fingers, (c) left wrist, (d and e) bilateral shoulders, (f) left elbow, and (g) left femur. Orange arrows represent acral osteolysis that affected the distal phalanx of (a) right thumb, (b) right long finger, and (c) left index finger.
Tumoral calcinosis is characterized by extraosseous calcium deposits in periarticular soft tissue regions. Lesions may be asymptomatic or cause local pain, ulceration, and neurovascular symptoms due to compression with risk of secondary infections.1 Typically, the lesions are in the periarticular regions, especially around the shoulder, hip, elbow, and wrist. Primary forms occur due to excess phosphate reabsorption in the kidney secondary to mutations in genes involving proteins that promote phosphate excretion, for example, FGF23, GALNT3, and KL.2 Secondary tumoral calcinosis occurs due to abnormal metabolism of phosphorous and/or calcium. Prevalence rates are 3% in patients with ESKD with the most important risk factor being hyperphosphatemia. Treatment options include improving serum phosphate level with diet modification, non-calcium-based phosphate binders, for example, sevelamer or ferric citrate, avoiding vitamin D analogues, use of cinacalcet to improve serum PTH and calcium, and improving phosphate clearance with effective hemodialysis (increased frequency or duration) or peritoneal dialysis (using a long dwell). Using a low calcium bath is an effective way of controlling the serum calcium level. Other treatment options that have shown efficacy include parathyroidectomy and sodium thiosulfate.3,4
Conflicts of interest
There are no conflicts of interest.
References
- Tumoral calcinosis: Diffuse multifocal form in hemodialysis patients. Two case reports. Orthop Traumatol Surg Res. 2017;103:815-20.
- [Google Scholar]
- A 23-year-old patient with secondary tumoral calcinosis: Regression after subtotal parathyroidectomy: A case report. Int J Surg Case Rep. 2016;23:56-60.
- [Google Scholar]
- Sodium thiosulphate treatment of uraemic tumoral calcinosis. Rheumatology (Oxford). 2014;53:547-51.
- [Google Scholar]






