Translate this page into:
Hand Grip Strength in Patients on Maintenance Hemodialysis: An Observational Cohort Study from India
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Malnutrition is a common manifestation in patients with dialysis and is a major cause of mortality in these patients. Various biochemical parameters are used to detect and monitor malnutrition in these patients. Confounding variables present in hemodialysis have an effect on the sensitivity and specificity of these tests.
Methods:
We studied hand grip strength (HGS) as a monitoring tool for protein malnutrition in these patients.
Results:
In a prospective observational study over 18 months, 83 patients (60 males) consented to be part of the study. The biochemical parameters showed the mean (±sd) of haemoglobin and albumin as 10.(±1.9) gm/dl and 3.5 (±0.5) gm/dl respectively. Majority of the patients (54/83) were well nourished according to subjective global assessment (SGA). The hand grip score in the cohort was weak in the majority of patients. It is interesting to note that majority of the males have weak HGS as compared with the general population of the same age group. The female patients had HGS which were in the normal range of values that of the population. A multiple regression analysis showed that there was a significant association with serum creatinine and HGS.
Conclusions:
No correlation between albumin and HGS was noted. Of the anthropometric variables a significant correlation was noted between mid arm muscle circumference and HGS.
Keywords
Anthropometry
hand grip strength
hemodialysis
malnutrition
Introduction
Malnutrition is a common complication and has prognostic implications in patient on maintenance hemodialysis.[1] The cause of malnutrition in maintenance hemodialysis patient is multifactorial and includes inadequate food intake, hormonal and gastrointestinal disorders, dietary restrictions, drugs that affect nutrient absorption, insufficient dialysis and presence of associated comorbidities. Two types of malnutrition have been described in hemodialysis population; defective nutrition due to poor nutrition intake (true malnutrition) and an abnormal body composition with a reduction of somatic and visceral protein pool as a result of catabolic condition linked to a pro-inflamatory state.[2] Malnutrition has an important clinical implication in dialysis patients because it is a powerful predictor of morbidity and mortality.[3] As malnutrition is associated with poor prognosis, nutritional evaluation and appropriate intervention has been recognized as an important therapeutic approach for patients on hemodialysis.[4] Many evaluation parameters (anthropometry, laboratory investigations etc) are utilised in the assessment of these patients. We present our data of nutritional assessment with the use of the hand grip strength and correlate it with commonly used nutritional parameters and indices.
Materials and Methods
A cross-sectional observational study was conducted in our hemodialysis unit between July 2016 and December 2017. All patients who were initiated on dialysis and who consented for the study were included. The general demographic details (age, gender, comorbidities), clinical evaluation (edema, skin changes of malnutrition etc) dialysis details (duration, frequency, vintage), dietary history (24 hour recall), anthropometric evaluation, (height, weight, body mass index, triceps skin fold thickness (TSF), mid arm muscle circumference (MAMC) and hand grip strength (HGS)), and laboratory investigations (hemoglobin, total leucocyte count, creatinine, urea, potassium, albumin, serum transferrin, and serum iron) were noted. In all patients the subjective global assessment (SGA) score was calculated based on history and physical examination.[5]
All anthropometric measurements were done in the non fistula arm pre-dialysis as there are concerns of bleeding if the patient overexerts. The hand grip strength (HGS) was measured with the patient seated with the elbow flexed at 90 degrees and the forearm in the neutral position. Three measurements were taken and the best reading was noted for the study. The mechanical dynamometer (Harpenden and Smedley) was used. The patients self adjusted the dynamometer depending on their hand size.[6] Anthropometric measurements were done in all patients. Triceps skin fold thickness was done with calipers and mid arm circumference was measured with a stretchable tape.[7]
The mid arm muscle circumference was done using the following formula:
MAMC = MAC (cm)-π TSF (mm)/10.
Subjective global assessment was used to assess the nutritional status of the cohort. A six point score was applied on the 5 variables tested and the group was classified into well nourished (score 7-14), mild to moderately malnourished (score 15-35) and severely malnourished (score 36-49).
The demographoic, laboratory and anthropometric variables were reported as mean (±sd.). A multiple regression analysis was done to look for significant association between HGS and various laboratory and anthropometric variables. The correlations between hand grip and laboratory variables (hemoglobin, total lymphocyte count, creatinine, albumin, serum iron, total iron binding capacity) and anthropometric variables (BMI, triceps skin fold thickness, mid arm muscle circumference) were analysed. All statistical analyses was done with SPSS Version 21 (IBM, Armonk, NY USA). A P value of <0.05 was considered significant.
Results
A total of 83 patients consented for the study. No patient refused to undergo anthropometric testing and no patient was excluded because of inability to correctly use the dynamometer. Of the 83 subjects, 60 were men. The mean age was 56.2 ± 12.6 years. Of the 83 patients, there were 24 patients who were aged 60 years and above, 7 patients were 70 years and above and 3 were 80 years and above. The youngest in the cohort was 15 years of age and the oldest patient on dialysis was 85 years. There were 42 (29 males and 13 females) patients whose primary diagnosis was type 2 diabetes mellitus. Sixty-nine patients were dialysed with an arteriovenous fistula and the rest had permanent internal jugular catheters. The biochemical and anthropometric parameters of the cohort are given in Table 1. The mean haemoglobin in the cohort was more than 10 gm/dl and the mean serum albumin in the cohort was 3.5 g/dl. In SGA score, majority of the patients (n = 54) fell in the well nourished group. This cohort is from a tertiary care hospital catering for paying patients and patients with medical insurance (patients from a relatively higher socioeconomic group) and the results are similar to that of a recent study from a tertiary care hospital in India.[8] Most of the midarm muscle circumference (MAMC) and triceps skin fold (TSF) thickness measurements fall in the standard well nourished group. The average value for MAMC and TSF are standardised and easy to compare,[9] however very little literature exists on hand grip score in hemodialysis patients.
| Laboratory parameter | Value | Range |
|---|---|---|
| Haemoglobin (g/dl) | 10.2±1.9 | 13-17 |
| Creatinine (mg/dl) | 7.7±2.5 | 0.52-1.04 |
| Urea (mg/dl) | 85.2±28.1 | 15-36 |
| Albumin (g/l) | 3.5±0.5 | 3.5-5.1 |
| TLC (cell/cumm) | 7496.2±2365.1 | 4000-11000 |
| Serum Iron (µg/dl) | 76.1±36.05 | 60-170 |
| MAMC (cm) | 25.7±4.01 Males: 27.8±5.7 Females: 24.9±2.8 |
Male-17.6-29.3 Female-17.1-28.5 |
| Triceps Skin fold thickness (cm) | 19±6.4 Males: 16.9±4.2 Females: 24.6±7.8 |
Male-7.5-12.5 Female 9-16.5 |
| Hand grip score (kg) | 20.9±4.1 Males: 21.1±4.3 Females: 20.6±3 |
Male-<35.5-Weak>54.5 Strong Female <18.9 Weak>32.4 strong* |
In males, the hand grip was done in the dominant arm in 51 (85%) patients and in females, it was done in 18 (78.2.%) It is interesting to note that majority of the males have weak HGS as compared with the general population of the same age group. Interestingly some of the female patients had HGS which were in the normal range of values that of the population.[10] Unfortunately there are no normative data from India. Female patients in the cohort were not on dilaysis as long as the male patients were in our study. Mean dialysis duration in females was 36.6 months vs 46.6 months in the male hemodialyis patients. In our cohort hand grip strength was significantly associated with dialysis vintage. Longer the duration the patient was on dialysis, the weaker the HGS [Figure 1]. The correlation of Hand grip and dialysis vintage was significant. This finding may explain the better handgrip strength in females in our study cohort. There is data in general population that HGS differs between dominant and non dominant arm. In our study HGS was measured in 14 patients, which was in the non dominant arm. The hand grip strength measurement was also analysed based on the gender and dominance and the data is given in Table 2.
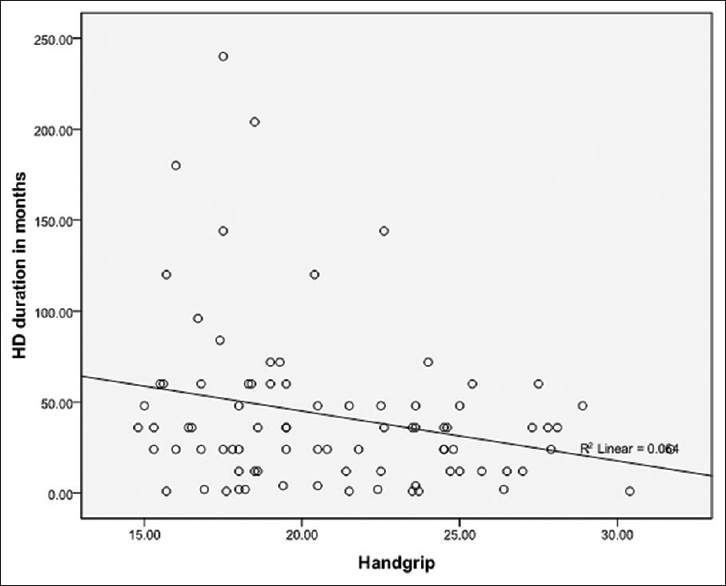
- The correlation between Hand grip strength (x axis) and dialysis vintage. Significant correlation between Hand grip strength and duartion of dialysis is noted (P = 0.022)
| Hand Grip Strength (kg) | Dominant | Non Dominant | P |
|---|---|---|---|
| Male (n=60) Dominant (n=51) Non Dominant (n=9) |
22.4 (±5.3) | 20.9 (±4.1) | 0.44 |
| Female (n=23) Dominant (n=18) Non Dominant (n=5) |
20.6 (±3.5) | 20.3 (±4.6) | 0.87 |
Pearson correlation analysis showed that there was a significant association with serum creatinine and mid arm muscle circumference. [Table 3]. There was significant correlation between HGS and serum creatinine and MAMC [Figure 2a and b]. Although the correlation between hand grip strength and creatinine is significant, which can be explained by the association of protein wasting underlying these two investigative variables, other factors may also contribute for this association. Statistically these factors are responsible for a small fraction of variability in HGS.
| Parameter | Pearson correlation | Sig. (2-tailed) |
|---|---|---|
| Hemoglobin | 0.123 | 0.277 |
| Total Lymphocyte Count (TLC) | 0.195 | 0.109 |
| Serum Creatinine | 0.263 | 0.018 |
| Serum Albumin | 0.226 | 0.056 |
| Serum Iron | 0.092 | 0.465 |
| Total Iron Binding Capacity (TIBC) | 0.050 | 0.695 |
| Body Mass Index (BMI) | 0.190 | 0.085 |
| Triceps Skin Fold Thickness (TSF) | 0.157 | 0.157 |
| Mid arm Muscle Circumference (MAMC) | 0.294 | 0.007 |
Bold value is significant <0.05

- (a) Correlation between serum creatinine (x axis) and hand grip (y axis). (b) Correlation between MAMC (x axis) and hand grip (y axis)
Discussion
Malnutrition in dialysis patients is categorised as a form of reduction in both protein and energy stores -protein energy wasting (PEW).[11] It is relatively common in patients on dialysis. The prevalence in various studies have been reported between 20 to 60% using SGA scores.[12] A recent study from a tertiary care hospital from India reported a prevalence of 32%.[8] Our cohort, similar to that of the Indian study, reported a prevalence of 29%. There were no patients with severe malnutrition.
Various measures including biochemical parameters, anthropometry, malnutrition scores (SGA, MIS), bioimpedance, has been extensively used a tool for detecting malnutrition. Commonly used biochemical parameters like albumin, haemoglobin, transferrin, prealbumin are useful in identifying high risk patients but are confounded by various other factors like inflammation, chronic liver disease, iron deficiency anemia etc.[13] Elaborate methodologies like bioimpedance are expensive and not available in all centres. The practical use of these methodologies is a major issue in our country.[9] Malnutrition indices are increasingly being used in hemodialysis patients. SGA and malnutrition inflammation score (MIS) are the two most common tools for evaluation in hemodialysis patients. The modified 7 point scale of SGA first used in the CANUSA study validated its prognostic significance [14] and is recommended in the diagnosis of malnutrition by NKF-DOQI and European Best Practice guidelines (EBPG) on nutrition.[15] SGA correlates well with various nutritional markers in many studies,[16] but its ability to diagnose degrees of malnutrition is not clear.[17] Some studies have raised questions about its value in hemodialysis patients. In a study of 76 patients there was significant lack of correlation between nitrogen index and SGA scores. The authors contend that significant caution should be exercised when SGA alone is used as a tool for evaluating malnutrition in hemodilaysis patients.[18] The importance of inflammation and its prognostic impact on cardiovascular mortality, infections and malnutrition is often overlooked in hemodialysis patients. This is addressed with MIS score.[19] However, most of these scores are subjective, have arbitrary cut offs (may not be valid in all ethnic groups) and have considerable inter and intra-observer variability. To overcome all this, a combined evaluation of both subjective and objective parameters is preferred.[5]
It is also being increasingly recognised that protein catabolism is significant in hemodialysis patients because of the underlying inflammation.[2021] For the evaluation of protein deficit and catabolism, evaluation of muscle function is useful. Hand grip is a simple and reliable method of evaluation of muscle function and correlates with anthropometric and laboratory measurements of PEW. The functional status of general muscle strength is correlated consistently with the extent of the handgrip strength (HGS) and is routinely utilised as a function of skeletal muscle strength and function in nutritional evaluation of the general population.[22] The same concept is used in hemodialysis patients as the test is simple, fast, inexpensive and easy to perform.[23] Hand grip strength has also been shown to correlate well with malnutrition inflammation score.[24] As hand grip strength can be studied regularly and frequently this test can be used to detect early changes in nutritional status and allow appropriate intervention expeditiously.
Our study in a cohort of 83 stable patients on dialysis, the malnutrition prevalence with subjective global assessment was 35%, which is comparable with other Indian studies. The hemoglobin and the serum albumin levels were not very low as has been reported in earlier studies. The hand grip strength in the cohort was uniformly low in all the patients as seen in other studies except in the females in the age group of 45 years and above. Unfortulately, we did not have any female patient in the lower age group to comment whether the HGS is better in the female dialysis cohort in our part of the world. Understanding the correlation between hand grip strength and other biochemical parameters, it was found that significant correlation exists with serum creatinine and mid arm muscle circumference. Positive correlation between creatinine and a stronger hand grip strength is suggestive of a better nutritional status in these individuals. Significant correlation between MAMC and hand grip is expected as both indicate muscle function and protein metabolism. There was a trend to significant correlation between serum albumin also in our study. Current studies have critiqued the use of albumin as a nutritional marker in chronic kidney disease patients and in our population it is more a marker of inflammation than nutrition.[25]
There are a few limitations in our study. Firstly, it is a small observational cohort where hand grip is studied as a anthropometric parameter of malnutrition. This study does not give any information about the association between hand grip and inflammation which it was not intended to do. Finally, hand grip strength varies between dominant and non dominant hand. Majority of the testing was done in the dominant hand which also was the non fistula arm. In 14 patients the fistula was in the dominant arm, hence the HGS was noted in the non dominant arm. This was owing to the apprehension of any procedure being done in the fistula arm other than dialysis in this cohort. Anticipating concerns, we designed our study accordingly and the HGS was done in the non fistula arm irrespective of the dominance of the arm. It is important to note that there was no significant difference between the dominant and non dominant arm measurements. There are many studies which have elaborated the correlation between hand grip and inflammation and mortality. Our study was more to understand the value and limitations of this antropometric tool in detecting and monitoring protein malnutrition.
Despite all our limitations, this study, one of the earliest from a resource poor setting looks into the relevance of hand grip strength as a reliable, inexpensive objective tool in the study of malnutrition in our dialysis patients. In our dialysis units, trained human resource is scarce and applying SGA frequently as a monitoring tool is cumbersome. Also there is tremendous variability in the results which has to be interpreted appropriately. This study tries to emphasise the utility of a objective tool which can not only detect protein wasting early but can help us in regular monitoring so that timely interventions are instituted in our at risk patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Predictors of mortality in haemodialysis patients. J Am Soc Nephrol. 1992;3:1613-22.
- [Google Scholar]
- Malnutrition: A frequent misdiagnosis for hemodialysis patients. J Clin Invest. 2002;110:437-9.
- [Google Scholar]
- Mortality risk in hemodialysis patients and changes in nutritional indicators: DOPPS. Kidney Int. 2002;62:2238-45.
- [Google Scholar]
- Handgrip strength, lean body mass and plasma proteins as markers of nutritional status in chronic kidney disease close to start of dialysis therapy. Am J Kidney Dis. 2000;36:1213-25.
- [Google Scholar]
- Applicability of subjective global assessment and malnutrition inflammation score in the assessment of nutritional status on chronic kidney disease. J Bras Nefrol. 2014;36:236-40.
- [Google Scholar]
- Handgrip strength and its dialysis determinants in hemodialysis patients. Nutrition. 2011;27:1125-9.
- [Google Scholar]
- Handgrip strength is an independent predictor of renal outcomes in patients with chronic kidney diseases. Nephrol Dial Transplant. 2011;26:3588-95.
- [Google Scholar]
- Impact of malnutrition, inflammation, and atherosclerosis on the outcome in hemodialysis patients. Indian J Nephrol. 2017;27:277-83.
- [Google Scholar]
- Evaluating the accuracy of nutritional assessment techniques applied to hospitalised patients: Methodology and comparisons. J Parenter Enteral Nutr. 1984;8:153-9.
- [Google Scholar]
- Hand grip strength; age and gender stratified normative data in a population-based study. BMC Res Notes. 2011;4:127-31.
- [Google Scholar]
- A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int. 2008;73:391-8.
- [Google Scholar]
- Subjective global assessment of nutritional status is strongly associated with mortality in chronic dialysis patients. Am J Clin Nutr. 2009;89:787-93.
- [Google Scholar]
- Routine protein energy supplementation in adults: Systematic review. Br Med J. 1998;317:495-501.
- [Google Scholar]
- Adequacy of dialysis and nutrition in continuous peritoneal dialysis: Association with clinical outcomes. Canada-USA (CANUSA) peritoneal study group. J Am Soc Nephrol. 1996;7:198-207.
- [Google Scholar]
- National Kidney Foundation/Kidney Disease Outcome Quality Initiative: Clinical Practice Guidelines for nutritionin children with chronic kidney disease: 2008 Update. Am J Kidney Dis. 2009;53(Suppl 2):S1-S123.
- [Google Scholar]
- Comparison of different assessments for evaluating malnutrition in Chinese patients with end-stage renal disease with maintenance hemodilaysis. Nutr Res 2012:266-71.
- [Google Scholar]
- Validity of subjective global assessment as a nutritional marker in end stage renal disease. Am J Kidney Dis. 2002;40:126-32.
- [Google Scholar]
- Is subjective global assessment a reliable measure of nutritional status in hemodialysis? J Ren Nutr. 2004;14:26-30.
- [Google Scholar]
- A malnutrition -inflammation score is correlated with morbidity and mortality in maintenance hemodialysis patients. Am J Kidney Dis. 2001;38:1251-63.
- [Google Scholar]
- Systemic inflammation is associated with exaggerated skeletal muscle protein catabolism in maintenance hemodialysis patients. JCI Insight. 2017;2:e95185. doi: 10.1172/jci.insight. 95185
- [Google Scholar]
- Muscle atrophy, inflammation and clinical outcome in incident and prevalent dialysis patients. Clin Nutr. 2008;27:557-64.
- [Google Scholar]
- Hand grip strength test and its use in nutritional assessment. Rev Nutr. 2008;21:223-5.
- [Google Scholar]
- Hand-Grip muscle strength, lean body mass, and plasma proteins as markers of nutritional status in patients with chronic renal failure close to start of dialysis therapy. Am J Kid Dis. 2000;36:1213-25.
- [Google Scholar]
- Malnutrition-inflammation score is associated with handgrip strength in non dialysis dependant chronic kidney disease patients. J Ren Nutr. 2013;23:283-7.
- [Google Scholar]







