Translate this page into:
Hypercalcemia in Immunocompromised Hosts: Think of the Unlikely
Corresponding author: Kalathil K Sureshkumar, Division of Nephrology and Hypertension, Medicine Institute, Allegheny General Hospital, Allegheny Health Network, Pittsburgh, PA, United States. E-mail: kalathil.sureshkumar@ahn.org
-
Received: ,
Accepted: ,
How to cite this article: Sureshkumar KK, Conant A, Nashar K. Hypercalcemia in Immunocompromised Hosts: Think of the Unlikely. Indian J Nephrol. doi: 10.25259/IJN_165_2025
Dear Editor,
Hypercalcemia has a varied etiology, with treatment choice dictated by the underlying cause. We present an immunocompromised host with weight loss, lymphadenopathy, and hypercalcemia masquerading as malignancy.
A 74-year-old male with successful liver transplantation, maintained on tacrolimus and mycophenolic acid (MPA) along with standard infection prophylaxis, presented 4 months later with constitutional symptoms and 20-pound weight loss. The corrected calcium was 11.9 mg/dL (8.4-10.3). Computed tomography showed mediastinal and bilateral axillary lymphadenopathy. Serum Epstein-Barr Virus (EBV) and Cytomegalovirus (CMV) PCR were negative. Hypercalcemia work-up revealed intact parathyroid hormone (6.8 pg/mL; 11.0-68.0), 25-hydroxy vitamin D (44.6 ng/mL; 30-100), and ĸ/λ light chain ratio (1.45; 0.26-1.65). M-spike was absent on serum protein electrophoresis. Blood culture grew Cryptococcus neoformans. Serum Cryptococcal antigen titer was positive (1:4096). Lumbar puncture revealed CSF lymphocytic pleocytosis and positive cryptococcal antigen titer (1:32). Axillary lymph node biopsy showed cryptococcal lymphadenitis with diffuse involvement by encapsulated yeast forms within non-necrotizing granulomatous inflammation [Figure 1]. MPA was stopped. The patient was initiated on induction treatment with intravenous liposomal amphotericin B and oral flucytosine and continued for 2 more weeks after negative blood cultures, followed by 8 weeks of consolidative therapy with oral fluconazole. Hypercalcemia resolved a week after initiating antifungal therapy. The patient was continued on maintenance fluconazole and was doing well.
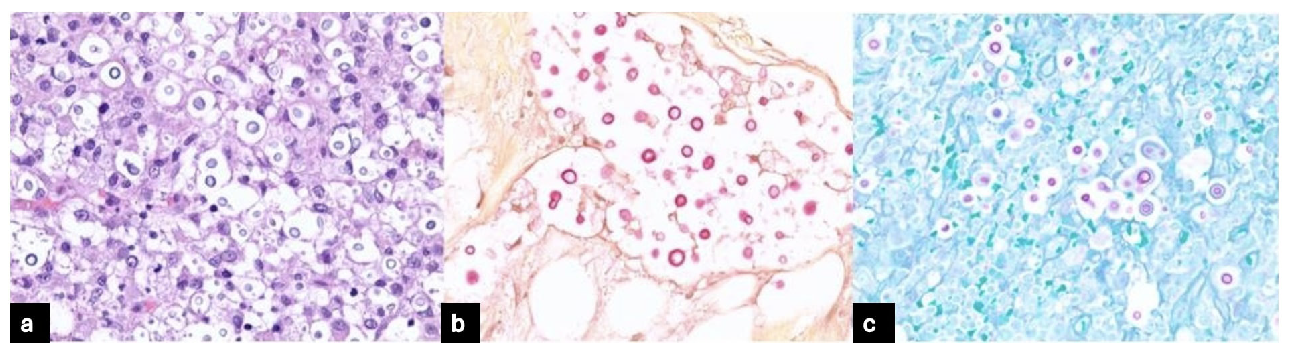
- (a) H&E stain showing lymphoid material replaced by granulomatous inflammation with predominance of yeast forms (x100). (b) Mucicarmine stain showing yeast forms (x100). (c) Periodic Acid Schiff stain showing yeast forms (x100). H&E: Hematoxylin and eosin.
Hypercalcemia is a rare disseminated and granulomatous fungal infection manifestation, particularly in immunocompromised individuals.1 The exact etiology is unclear, but enhanced and localized 1-α hydroxylase activity from macrophages, with increased 1, 25-di (OH) vitamin D production is implicated.2 Osteotropic substance resembling humoral hypercalcemia of malignancy and osteopontin, a macrophage and osteoclast activator are also implicated.3,4 Weight loss and lymphadenopathy in our immunosuppressed patient raised concern for malignancy. However, blood culture and lymph node histology clinched the diagnosis, enabling prompt therapy with resolution of the symptoms and hypercalcemia.
Acknowledgement
Presented as a poster during American Society of Nephrology Virtual Kidney Week 2021.
Conflicts of interest
There are no conflicts of interest.
References
- Refractory hypercalcemia associated with disseminated Cryptococcus neoformans infection. Endocrinol Diabetes Metab Case Rep. 2021;2021:20-0186.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Endocrine and metabolic manifestations of invasive fungal infections and systemic antifungal treatment. Mayo Clin Proc . 2008;83:1046-60.
- [CrossRef] [PubMed] [Google Scholar]
- Hypercalcemia associated with infection by Cryptococcus neoformans and Coccidioides immitis. Am J Med Sci. 1999;318:419-23.
- [CrossRef] [PubMed] [Google Scholar]
- Osteopontin is strongly expressed by histiocytes in granulomas of diverse etiology. Lab Invest. 1997;77:103-8.
- [PubMed] [Google Scholar]






