Translate this page into:
Hypermanganesemia in Patients with Hyperintensity in Basal Ganglia with Ongoing Maintenance Hemodialysis
Address for correspondence: Dr. Topoti Mukherjee, Department of Nephrology, Manipal Hospital Whitefield, # 143, 212-215, EPIP Industrial Area, Hoodi Village, KR Puram, Hobli, Bengaluru - 560 066, Karnataka, India. E-mail: drtopoti@gmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Dear Sir,
Subtle changes in trace elements are not well studied in patients with end-stage renal disease. In the present study, we encountered two cases of incidentally detected hypermanganesemia in patients with chronic hemodialysis between July 2018 and December 2018. In the first case, a 55-year-old woman presented with a severe headache and normal neurological examination. MRI brain showed bilateral hyperintensity of the globus pallidus on T1-weighted images [Figure 1]. Serum manganese was 31.8 μg/L (normal range 4.2 to 16.5 mcg/L). In the second case, a 53- year- old woman presented with sudden onset blindness and high blood pressure. Ophthalmological examination was normal, suggestive of cortical blindness. MRI imaging showed hyperintensities in the parieto-occipital areas, with altered signal intensities in the globus pallidus and substantia nigra on T1-weighted images [Figure 2]. A diagnosis of posterior reversible encephalopathy syndrome (PRES) was entertained. The vision dramatically improved with steroids and control of the blood pressure. Steroids were given for the benefit of the doubt as her native disease was antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis. Serum manganese level was high (21.9 μg/L).
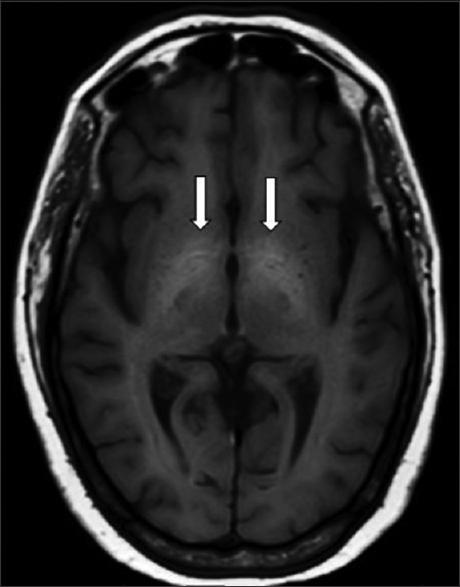
- Bilateral hyperintensity of globus pallidus on T1-weighted images on MRI
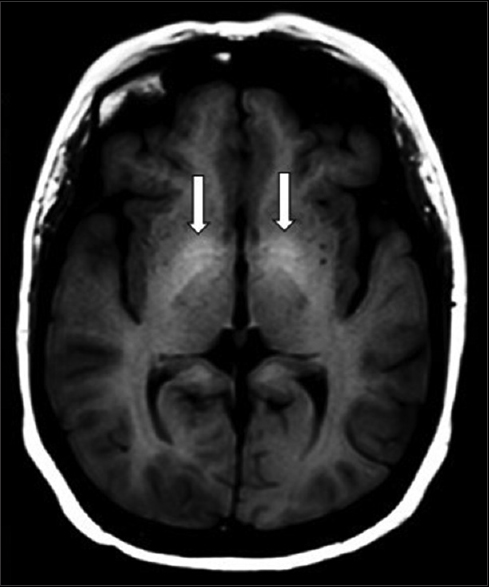
- Bilateral hyperintensities in parieto-occipital areas, with altered signal intensities in the globus pallidus, and substantia nigra on T1-weighted images
Manganese (Mn) is an essential nutrient for intracellular activities and several biological functions.[1] It is used in agriculture, medicine, food, and leather industries.[1] Excessive Mn gets deposited in the brain, liver, kidney, pancreas, and bone, the brain being the main target. Dystonia and parkinsonian symptoms have been reported with hypermanganesemia,[23]often termed as manganese madness or manganism. The recommended dietary allowance of Mn is approximately 2.3 to 8.8 mg/day on a western diet.[4]Around 3–5% is absorbed in the gut. Excretion is by the gut, urinary excretion being negligible.[5]
There is a paucity of data on serum Mn levels in hemodialysis patients. Low levels, presumably due to removal through dialysis,[5] as well as high levels due to an increase in ultrafiltrable Mn have been reported.[6]Mykola et al. analyzed several trace elements in 41 patients on dialysis and 61 healthy controls. They found that Mn levels increased by 3.36 times in patients on hemodialysis as compared to healthy volunteers.[7] Besides, Mn toxicity due to contamination from the dialysate has been reported.[8] Ohtake et al. reported a case of Mn induced Parkinsonism in a patient on maintenance hemodialysis, who was on a health supplement (chlorella extract) containing 1.7 mg of Mn.[3]Brain is most susceptible to Mn intoxication, characterized by hyperintense areas on T1-weighted sequences in the basal ganglia. Apart from patients on hemodialysis, this has been seen in parenteral nutrition, portosystemic encephalopathy, carbon monoxide poisoning, and has also been reported in welders.[2] The differential diagnosis of high signal intensity on T1-weighted MR images includes paramagnetic substances such as Mn, methemoglobin, melanin, and copper. Other differentials include calcification, laminar necrosis in cerebral infarction, neoplasms, and hamartomas. All these conditions show low or normal signal intensity on T2-weighted images.[9] Serum Mn levels in our patients were sent in retrospect, after reviewing the literature of an association of these MRI findings in patients on maintenance hemodialysis.[2] The cause of high Mn levels in our patients is difficult to elucidate. In both our patients, MR imaging was ordered for evaluating the cause of the presenting symptom, and this was an incidental finding. Their dietary consumption was normal or marginally high (3 mg/day and 9 mg/day, respectively). There was no ingestion of oral supplements containing Mn. The degree of accumulation of the non-protein-bound Mn may partially explain the high levels. Concomitant dialysate levels of Mn were not sent as the standard dialysate does not contain Mn. Repeat Mn levels or neuroimaging were not done as it was not clinically warranted. We do not intend to attribute the symptoms or neurological findings to the elevated Mn levels. Awareness of this probable association may help further in optimizing the care of patients on maintenance hemodialysis.
Declaration of patient consent
The author certify that he has obtained appropriate patient consent. Patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- A preliminary study revealing a new association in patients undergoing maintenance hemodialysis: Manganism symptoms and T1 hyperintense changes in the basal ganglia. Am J Neuroradiol. 2007;28:1474-9.
- [Google Scholar]
- Manganese- induced Parkinsonism in a patient undergoing maintenance hemodialysis. Am J Kidney Dis. 2005;46:749-53.
- [Google Scholar]
- Manganese toxicity upon overexposure: A decade in review. Curr Environ Health Rep. 2015;2:315-28.
- [Google Scholar]
- Role of manganese in chronic hemodialysis patients. Int J Artif Organs. 1987;10:14-6.
- [Google Scholar]
- Trace metals protein binding in normal and dialyzed uremic serum. Trans Am Soc Artif Intern Organs. 1980;26:133-8.
- [Google Scholar]
- Disturbances of trace element metabolism in ESRD patients receiving hemodialysis and hemodiafiltration. Cent European J Urol. 2013;66:472-6.
- [Google Scholar]
- Acute manganese intoxication and pancreatitis in a patient treated with a contaminated dialysate. CMA J. 1982;126:503-5.
- [Google Scholar]






