Translate this page into:
Impact of Noncommunicable Diseases and Heat Stress on Estimated Glomerular Filtration Rate in Security Officers at a Tertiary Care Hospital in South India
Corresponding author: Elenjickal E. John, Department of Nephrology, Christian Medical College, Vellore, Tamil Nadu, India. E-mail: sonyjohn84@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: John EE, Valson AT, George R, Grace PJ, Anthony P, Jose N, et al. Impact of Noncommunicable Diseases and Heat Stress on Estimated Glomerular Filtration Rate in Security Officers at a Tertiary Care Hospital in South India. Indian J Nephrol. 2025;35:243-52. doi: 10.25259/ijn_386_23
Abstract
Background:
The job profile of security officers in tropical countries involves prolonged standing in hot conditions causing heat stress as well as complications of sedentary lifestyle. The objectives of this study were to estimate the prevalence of noncommunicable diseases and heat stress in security officers and analyze factors affecting heat stress and estimated glomerular filtration rate (eGFR).
Materials and Methods:
This was an observational cross-sectional study conducted among security personnel working at a tertiary care hospital in South India during the hottest months of March to May 2020. Screening camps were conducted during which anthropometric measurements were taken and blood was collected for hemoglobin, creatinine, and fasting glucose estimation. Urine dipstick analysis for glucose, protein, pH, and red and white blood cells were done on early morning voided sample. Heat stress was assessed by a validated 18-item questionnaire called heat strain score index (HSSI). A structured questionnaire was prepared for surveillance of risk factors of noncommunicable diseases.
Results:
A total of 678 security officers were screened. Majority (659/678, 97.2%) were men and mean age of the cohort was 45.4 ± 9.2 years. Fifty-two percent (355/678) of participants were engaged in outdoor work for a median duration of 6 (IQR, 0-8) hours/day. Prevalence of obesity, diabetes, hypertension, and chronic kidney disease (CKD) were 70.9, 25.5, 15.9 and 1.3 percentage, respectively. Half of the cohort (324/678) had definite heat stress and 0.9% (6/678) developed CKD of undetermined etiology. Heat stress was higher in those working outdoors and longer employment duration and lower in those with abdominal obesity. eGFR was lower in older officers, smokers, hypertensives, and those with longer employment duration, but was unaffected by HSSI scores.
Conclusion:
Kidney function was unaffected by high levels of heat stress experienced by security personnel working at a tertiary hospital in South India. Future studies are needed to understand the pathomechanisms of differential impacts of heat stress on kidney function of agricultural various worker categories.
Keywords
Chronic kidney disease
Diabetes
Glomerular filtration rate
Heat stress
Obesity
Security officers
Introduction
The job profile of security officers involves prolonged period of standing which results in complications of sedentary lifestyle. A high prevalence of diabetes, hypertension, dyslipidemia, obesity, and metabolic syndrome is reported among police personnel in India.1-3 In contrast, agricultural workers who carry out strenuous activities in hot climates are at risk of developing heat stress nephropathy.4 This form of occupational renal disease is known by various terminologies such as chronic interstitial nephritis in agricultural communities (CINAC), chronic kidney disease of nontraditional origin (CKDnt), and chronic kidney disease of undetermined etiology (CKDu). There is paucity of data on the prevalence of CKDu in occupations other than agricultural workers.5,6 Security officers from hot tropical climates are thus exposed to both traditional (diabetes, hypertension, obesity, dyslipidemia) and nontraditional (heat stress) risk factors of chronic kidney disease (CKD). However, the impact of these factors on kidney function has never been explored previously.
Vellore district in the state of Tamil Nadu has a tropical climate. The average annual temperature in Vellore is 26.9 degree Celsius (°C). The temperature is highest in the month of May [31.2 (26.2–37.4)°C] and lowest in December [22.5 (17.9–27.2)°C]. Heat stress is defined as metabolic plus environmental heat minus the heat dissipated from body to environment. There are about 165 different indices for measuring heat stress which are classified into environmental, physiological, perceptual, and perceptual-observational.7 Heat strain score index is a validated perceptual-observational heat stress index developed by Dehgan et al.8 This index has a Cronbach’s coefficient of 0.91 and all items have adequate factor loading of more than 0.40.9,10 It has been previously studied in miners, bakers, glass manufacturers, diesel power plant operators, petrochemical workers, municipal waste collectors, copper refinery and steel plant workers.11,12
Christian Medical College, Vellore, is a tertiary care hospital which spreads out across multiple campuses and involves around 700 security officers working under a single agency who were employed without a prior pre-employment medical checkup. The objectives of this study were
To estimate the prevalence of noncommunicable diseases such as diabetes, hypertension, obesity, and CKD among security officers employed at our tertiary care center.
To estimate prevalence of heat stress by HSSI.
To analyze factors affecting thermal stress.
To analyze the factors affecting estimated glomerular filtration rate (eGFR).
Materials and Methods
This was an observational cross-sectional study conducted at Christian Medical College, Vellore, Tamil Nadu, during the months of March to May 2020, which is the hottest period of the year. All security personnel, both men and women above 18 years of age working at various campuses were included in this study. Those who were employed for a duration of less than 6 months and those who did not consent were excluded from the study [Figure 1]. A structured questionnaire for data collection was prepared as per guidelines by World Health Organization (WHO) STEPwise approach to noncommunicable disease risk factor surveillance. This included demographic details (age, sex), co-morbidities (diabetes, hypertension, past kidney disease), working conditions (duration of employment, work-shift hours, site of work, outdoor work hours/day, water intake during work-shift), medications, addictions (smoking, alcohol intake), lifestyle, and family history [Supplemental File 1].
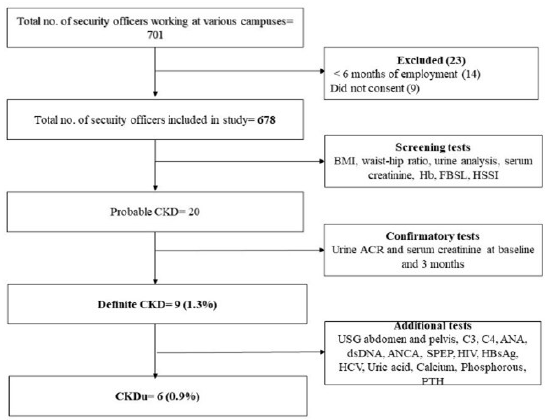
- Flowchart of recruitment of security personnel. ACR: Albumin to creatinine ratio, ANA: Antinuclear antibody, ANCA: Antineutrophil cytoplasmic antibody, BMI: Body mass index, C3: Complement component 3, C4: Complement component 4, CKD: Chronic kidney disease, CKDu: Chronic kidney disease of unknown etiology, dsDNA: Double-stranded deoxyribonuclease antibody, FBSL: Fasting blood sugar level, Hb: Hemoglobin, HCV: Hepatitis C virus antibody, HIV: Human immunodeficiency virus, HSSI: Heat strain score index, PTH: Parathyroid hormone, SPEP: Serum protein electrophoresis, USG: Ultrasound, HBsAg: Hepatitis B surface antigen.
Heat stress was assessed by an 18-item HSSI questionnaire which consisted of 12 observational and 6 perceptual questions [Supplemental File 2]. The questions were related to work-place setting, work-place ambient conditions, perceived symptoms at work, intensity of physical activity, body posture, and working attire. Scores for each item (primary score) were multiplied by effect coefficient of each question to get secondary scores. The secondary scores of each item were then summed to get a final score. Based on final HSSI scores, participants were classified into three zones:
Green or safe level (≤13.5) – no or low heat stress
Yellow or alarm level (13.6–18) – likelihood of heat stress
Red or danger level (>18) – definite heat stress (8)
This study was approved by institutional review board (IRB min no.12003, dated 24.04.2019) and written informed consent was taken from all participants.
Translation and back-translation of HSSI and data collection questionnaire
Both the questionnaires were translated to Tamil language according to guidelines for establishing cultural equivalency of instruments and outline of questionnaire development and translation process.13 The initial forward translation from English to Tamil was done separately by two independent translators who were well versed in both languages and also had a basic knowledge on occupational and environmental health. The Tamil version of questionnaire was then back translated to English by two different translators who did not have access to the original questionnaire. Pilot-testing was done among 100 security officers on World Kidney Day, 2019 [Supplemental Files 3 and 4].
Screening camps
Screening camps of 50–75 participants were conducted weekly for a period of 12 weeks. This was attended by physicians, nurses, dieticians, and laboratory and dialysis technicians. Rigorous training was provided to all personnel involved in data collection, sample collection, and anthropometric measurements. The security officers were briefed about the procedures a day before by the chief security officer. All participants were provided with ‘participant information sheet’ and a sterile container for urine analysis. Participants were taught how to collect midstream clean catch early morning urine sample and were asked to report at screening camp after an 8-hour overnight fast. The first morning void urine sample was preferred over a spot urine sample as the former is less influenced by factors like hydration and physical activity, thus reducing intra-individual variability.14
There were eight stations organized and manned by volunteers, students, and staff.
Station 1: After briefing the purpose of study, personal information was collected, written informed consent was taken, study participant number was allotted, and HSSI/data collection questionnaires were administered.
Station 2: Urine containers were collected and labeled correctly. Urine analysis for glucose, protein pH, red and white blood cells was done by a fully automated UC3500 urine chemistry analyzer using Meditape 10C (Sysmex corporation) urine strips by dipstick method.
Station 3: Weight, height, waist and hip circumference were measured as per WHO STEPS protocol.15 Weight was measured by a portable electronic weighing scale with an error of ± 0.1 kilogram (kg). Height was measured in centimeters (cm) by portable height measuring board. Waist and hip circumference were measured using 0.1 cm nonstretchable flexible tape over light clothing. Waist circumference was measured at the midpoint between the lower margin of last palpable rib and top of the iliac crest. Hip circumference was measured around the widest portion of the buttocks between the anterior superior iliac crests and the ischial tuberosities.
Station 4: Blood pressure (BP) was measured using a digital automatic BP monitor after the subjects were seated for 15 minutes as per WHO STEPS protocol.15 Small-, medium-, and large-sized cuffs were used for subjects with arm circumference 17–22, 22–32 and > 32 cm, respectively. Three BP measurements were taken and the mean of second and third readings was calculated.
Station 5: Blood was collected by trained technicians for fasting blood sugar level, hemoglobin, and creatinine.
Station 6: Brief medical examination was carried out by physicians and medications were optimized.
Station 7: Dietary counseling was provided by trained dieticians.
Station 8: Participants were seated and asked to complete both questionnaires. The questionnaires were crosschecked by volunteers for any blank items and errors.
Definitions
Impaired fasting glucose (IFG) and diabetes were defined as per classification of American Diabetes Association as fasting plasma glucose of 100–125 and ≥126 mg/dL, respectively.16 Hypertension was defined as per Joint National Committee (JNC 8) classification as systolic BP >140 mmHg and/or diastolic BP >90 mmHg.17 Past history of diabetes or hypertension was defined as an answer “yes” to the question “Have you been told by a doctor, nurse or health care worker that you have raised blood sugars or high blood pressure?” Overweight and obesity were defined as per consensus statement for Asian Indians as body mass index (BMI) of 23–24.9 and > 25 kg/m2, respectively. Abdominal obesity in males was defined as waist circumference >90 cm and/or waist–hip ratio >0.88. Abdominal obesity in females was defined as waist circumference >80 cm and/or waist–hip ratio >0.80.18
Nonvisible hematuria was defined as >5 red blood cells per high-power field. Pyuria was defined as >5 white blood cells per high-power field. Glycosuria and proteinuria were defined as urine dipstick result of ≥1+ for protein and glucose, respectively. Acidic and alkaline urine were defined as urine pH < 6 and >8, respectively. Albuminuria was graded based on urine albumin to creatinine ratio (mg/g) into normal (<30), moderately increased (30–300) and severely increased (>300). eGFR was calculated by Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula.19 “Probable CKD” was defined as eGFR < 60 mL/min/1.73m2 and/or urine dipstick result for protein ≥1+. “Definite CKD” was defined as eGFR < 60 mL/min/1.73 m2 with or without albuminuria > 30 mg/day on two occasions three months apart.20 CKDu was defined as CKD without recognizable cause such as diabetes, hypertension, glomerulonephritis, or genetic disease.
Follow-up procedures and outcomes
Participants who were newly detected to have hypertension, diabetes, or anemia were evaluated as per institutional protocol and treated as per physician discretion. All participants who were diagnosed as “probable CKD” underwent early morning urine albumin to creatinine ratio (ACR) estimation. A repeat serum creatinine and urine ACR was performed after 3 months. Those who were diagnosed as “definite CKD” were evaluated by a nephrologist to ascertain the etiology of CKD and were treated as per nephrologists’ discretion [Figure 1].
Statistical analysis
Data were presented as mean ± standard deviation (SD), or median [interquartile range (IQR)], or frequency (percentage) according to the types and distribution of variables. Differences among groups of normally distributed variables were analyzed by t-test or one-way ANOVA (factors affecting eGFR). Categoric variables were compared using Pearson’s chi-squared or Fisher’s exact test (factors affecting HSSI). Pearson correlation coefficient (r) was used to measure linear correlation between continuous variables like BMI, eGFR, and HSSI scores. The potential confounders of eGFR which were included in analysis were age, sex, duration of employment, diabetes, hypertension, nephrotoxic medication, obesity, smoking, and family history of kidney disease. Statistical analyses were performed using Statistical Package for Social Sciences software for Windows, version 21.0 (SPSS Inc., Chicago, IL), and graphs were made using Graph Pad Prism 7.0e (Graph Pad Software Inc., San Diego, CA). A p-value of <0.05 was taken as significant.
Results
A total of 678 security officers were screened over a period of 12 weeks. Majority (659/678, 97.2%) were men [Table 1]. Mean age of the cohort was 45.4 ± 9.2 years and 30.5% (207/678) were above 50 years. Thirteen percent (90/678) of officers were known diabetics and majority of them (68/90, 75.5%) were on oral anti-diabetic agents. Nine percent (59/678) of officers were known hypertensives and of these, 36 (61%) were on anti-hypertensive medications. Median duration of employment was 5 (IQR, 1–10) years and 25.7% (174/678) of officers were employed for >10 years. All participants had a fixed work-shift of 8 hours/day. Fifty-two percent (355/678) of participants were engaged in outdoor work for a median duration of 6 (IQR, 0–8) hours/day. Majority (421/678, 62.1%) of participants consumed an average of >2 L water during the 8-hour work shift. Water intake patterns did not differ with site of work or with HSSI category. Twenty-four percent (164/678) of officers gave history of frequent analgesic intake. Three percent (20/678) of officers were active smokers with a median exposure of 0.65 (IQR, 0.5–2) pack-years.
| Baseline characteristics | Entire cohort (n = 678) |
|---|---|
| Sex (n, %) | |
| Men | 659 (97.2) |
| Women | 19 (2.8) |
| Age, years | 45.4 ± 9.2 |
| Age > 50 years (n, %) | 207 (30.5) |
| Diabetes mellitus (n, %) | |
| Past history of diabetes | 90 (13.3) |
| Treatment for diabetes | |
| Diet | 20/90 (22.2) |
| Oral anti-diabetic agents | 68/90 (75.5) |
| Insulin | 2/90 (2.2) |
| Hypertension | |
| Past history of hypertension | 59 (8.7) |
| Anti-hypertensives yes (n, %) | 36/59 (61) |
| Working conditions | |
| Duration of employment, years, median (IQR) | 5 (1–10) |
| Site of work | |
| Indoor | 323 (47.6) |
| Outdoor | 132 (19.5) |
| Both | 223 (32.9) |
| Work-shift (hours/day) | 8 |
| Outdoor work (hours/day), median (IQR) | 6 (0–8) |
| Water intake during 8-hour work shift (n, %) | |
| <1 L | 81 (11.9) |
| 1–2 L | 176 (26) |
| >2 L | 421 (62.1) |
| Kidney disease (n, %) | |
| Past history of kidney disease | 24 (3.5) |
| Past history of kidney stone | 18 (2.7) |
| Past history of intake of nephrotoxic drugs | |
| Analgesics | 164 (24.2) |
| Complementary and alternative medicines | 18 (2.6) |
| Antacids | 35 (5.2) |
| Nocturia | 224 (33) |
| Addictions | |
| Smoking | |
| Reformed smoker (n, %) | 62 (9.1) |
| Active smokers (n, %) | 20 (2.9) |
| Pack-years, median (IQR) | 0.65 (0.5–2) |
| Alcohol intake yes (n, %) | 254 (37.5) |
| Frequency of alcohol intake (n, %) | |
| <Once a month | 100/254 (39.4) |
| 1–3 days/month | 89/254 (35) |
| 1–2 days/week | 40/254 (15.7) |
| 3–4 days/week | 14/254 (5.5) |
| 5–6 days/week | 3/254 (1.2) |
| Daily | 8/254 (3.1) |
| Lifestyle history (n, %) | |
| Exercise yes | 358 (52.8) |
| Cycling to work yes | 488 (72) |
| Extra salt in diet | |
| Never | 225 (33.2) |
| Rarely | 44 (6.5) |
| Sometimes | 280 (41.3) |
| Always | 50 (7.4) |
| Family history (n, %) | |
| Diabetes mellitus | 150 (22.1) |
| Hypertension | 78 (11.5) |
| Kidney disease | 16 (2.4) |
| Heart disease | 27 (4) |
IQR: Inter-quartile range.
Screening tests in security officers
Half of the cohort (348/678) were obese and another 22.6% (153/678) were overweight as per BMI classification [Table 2]. Abdominal obesity was seen in 58.3 (384/659) and 84.2 (16/19) percent men and women officers, respectively. Obesity was more common among diabetics (83.8% versus 77.2%, p = 0.084). Forty-nine (7.2%), 51 (7.5%), and 83 (12.2%) participants were newly detected to have hypertension, IFG and diabetes, respectively. Anemia was detected in 27 (4%) participants (23 men and 4 women). Mean eGFR of the cohort was 100.4 ± 14.2 mL/min/1.73 m2. Nine (1.3%) participants had eGFR <60 mL/min/1.73 m2. Proteinuria (by dipstick) was detected in 11/678 (1.6%) participants, of which 6 (54.5%) had diabetes. Acidic urine was detected in 494/678 (73.1%) participants, and occurred more commonly in those working outdoors [outdoors: 102/132 (77.9%) versus outdoors and indoors: 163/223 (73.4%) versus indoors: 229/323 (70.9%), p = 0.151] and in those consuming <2 L of water during the work-shift [<2L: 199/257 (77.4%) versus >2L: 294/421 (70.4%), p = 0.031].
| Screening test | Entire cohort (n = 678) |
|---|---|
| Anthropometry | |
| Body mass index, kg/m2 | 25.4 ± 3.8 |
| BMI category (n, %) | |
| Underweight | 13 (1.9) |
| Normal range | 170 (25.1) |
| Overweight | 153 (22.6) |
| Obese | 342 (50.4) |
| Waist circumference, cm | 80.9 ± 15.6 |
| Hip circumference, cm | 75.6 ± 16.1 |
| Waist-to-hip ratio | 1.14 ± 0.39 |
| Abdominal obesity (males) | |
| Waist circumference > 90 cm (n, %) | 235/659 (35.7) |
| Waist–hip ratio > 0.88 | 384/659 (58.3) |
| Either of the two | 384/659 (58.3) |
| Abdominal obesity (females) | |
| Waist circumference > 80 cm (n, %) | 15/19 (78.9) |
| Waist-hip ratio > 0.80 | 16/19 (84.2) |
| Either of the two | 16/19 (84.2) |
| Blood pressure | |
| Systolic BP, mmHg | 119.6 ± 15.9 |
| Diastolic BP, mmHg | 77.9 ± 9.5 |
| Newly detected hypertension (%) | 49 (7.2) |
| Prevalent cases of hypertension (%) | 108 (15.9) |
| Diabetes mellitus | |
| Fasting blood sugar level, mg/dL median (IQR) | 99.5 (91–114) |
| Newly detected diabetes mellitus (%) | 83 (12.2) |
| Newly detected impaired fasting glucose (%) | 51 (7.5%) |
| Prevalent cases of diabetes mellitus (%) | 173 (25.5) |
| Heat strain score index (HSSI) | |
| Scale of HSSI | 18 ± 6.4 |
| HSSI category n (%) | |
| Green zone | 179 (26.4) |
| Yellow zone | 175 (25.8) |
| Red zone | 324 (47.8) |
| Hemoglobin g/dL | 15.1 ± 1.6 |
| Anemia n (%) | 27 (4) |
| Kidney function | |
| Serum creatinine, mg/dL (range) | 0.9 ± 0.2 (0.1–2) |
| eGFR CKD-EPI, mL/min/1.73 m2 | 100.4 ± 14.2 |
| eGFR categories, mL/min/1.73 m2 (n, %) | |
| 90 | 547 (80.7) |
| 60–89 | 121 (17.8) |
| 30–59 | 8 (1.2) |
| 15–29 | 0 |
| <15 | 1 (0.1) |
| Urinalysis | |
| Glycosuria (n, %) | 133 (19.6) |
| Nonvisible hematuria (n, %) | 30 (4.4) |
| Leucocyturia (n, %) | 16 (2.4) |
| Proteinuria (n, %) | 11 (1.6) |
| pH | 5.8 ± 0.7 |
| Acidic urine (n, %) | 494 (73.1) |
| Alkaline urine (n, %) | 1 (0.1) |
BMI: Body mass index, BP: Blood pressure, CKD-EPI: Chronic kidney disease-epidemiology collaboration, eGFR: Estimated glomerular filtration rate, IQR: Inter-quartile range.
Heat strain score index
Mean HSSI score of the cohort was 18 ± 6.4. Twenty-six (179/678), 26 (175/678), and 48% (324/678) of officers were classified into green, yellow, and red zones, respectively. HSSI scores were higher in officers working outdoors (outdoor: 51.5% versus indoors: 43.7%) and those with a longer duration of employment (<5 years: 41.9% versus >5 years: 54.4%, p = 0.005). A positive correlation was observed between HSSI scores and duration of employment (r = 0.15, p < 0.001) and number of hours of outdoor work (r = 0.09, p = 0.022). HSSI scores were lower in those with abdominal obesity (42.8% versus 55%, p = 0.006) [Supplemental Table 1].
Factors affecting glomerular filtration rate
Mean eGFR was lower in men (men: 100.1 ± 14.2 versus women: 108.5 ± 11.3 mL/min/1.73 m2, p = 0.001), age > 50 years (93.9 ± 12.9 versus 103.2 ± 13.9 mL/min/1.73 m2, p < 0.001), hypertensives (97.4 ± 13.7 versus 100.9 ± 14.2 mL/min/1.73 m2, p = 0.019), longer duration of employment (>5 years: 98.5 ± 12.8 versus <5 years: 102 ± 15.2 mL/min/1.73 m2, p = 0.001), and smokers (nonsmokers: 100.1 ± 14.2 versus <10 pack-years: 103 ± 13.9 versus >10 pack-years: 93.1 ± 10.6 mL/min/1.73 m2, p = 0.097). However, women security officers were younger in age (36.2 ± 8.6 years) as compared to men (45.7 ± 9.1 years, p < 0.001). eGFR was unaffected by the presence of diabetes, BMI, site of work, duration of outdoor work-shift, and HSSI [Table 3, Figure 2]. No correlation was found between eGFR and HSSI scores as continuous variables (r—0.04, p = 0.29).
| Factor | Estimated glomerular filtration rate mL/min/1.73 m2 | p-value | ||
|---|---|---|---|---|
| Sex | ||||
| Men | 100.1 ± 14.2 | 0.001 | ||
| Women | 108.5 ± 11.3 | |||
| Age (years) | ||||
| <50 | 103.2 ± 13.9 | <0.001 | ||
| >50 | 93.9 ± 12.9 | |||
| Diabetes mellitus | ||||
| No | 100.5 ± 14.6 | 0.672 | ||
| Yes | 99.9 ± 12.8 | |||
| Hypertension | ||||
| No | 100.9 ± 14.2 | 0.019 | ||
| Yes | 97.4 ± 13.7 | |||
| Duration of employment | ||||
| <5 years | 102 ± 15.2 | 0.001 | ||
| >5 years | 98.5 ± 12.8 | |||
| Site of work | ||||
| Indoor | 100.6 ± 12.6 | 0.126 | ||
| Outdoor | 98.2 ± 16.9 | |||
| Both | 101.3 ± 14.5 | |||
| Heat exposure (hours per day) | ||||
| <5 hours | 100.5 ± 14.9 | 0.871 | ||
| >5 hours | 100.3 ± 13.5 | |||
| Water intake during work shift | ||||
| <1 L | 102.4 ± 13.7 | 0.366 | ||
| 1–2 L | 100.3 ± 14.6 | |||
| >2 L | 100 ± 14.1 | |||
| Past H/O kidney disease | ||||
| No | 100.4 ± 14.1 | 0.511 | ||
| Yes | 98.5 ± 17.8 | |||
| Past H/O kidney stones | ||||
| No | 100.4 ± 14.3 | 0.620 | ||
| Yes | 98.7 ± 10.7 | |||
| Past H/O nephrotoxic medications | ||||
| No | 100.4 ± 14.1 | 0.883 | ||
| Yes | 100.2 ± 14.4 | |||
| Nocturia | ||||
| No | 100.4 ± 14 | 0.831 | ||
| Yes | 100.2 ± 14.7 | |||
| Smoking | ||||
| No | 100.1 ± 14.2 | 0.294 | ||
| Reformed smokers | 103 ± 12.8 | |||
| Active smokers | 99.6 ± 17.2 | |||
| Pack-years of smoking | ||||
| Nonsmokers | 100.1 ± 14.2 | 0.097 | ||
| <10 pack-years | 103 ± 13.9 | |||
| >10 pack-years | 93.1 ± 10.6 | |||
| Alcohol intake | ||||
| No | 100.9 ± 13.6 | 0.189 | ||
| Yes | 99.4 ± 15.1 | |||
| Exercise | ||||
| No | 100.3 ± 14.6 | 0.434 | ||
| Yes | 101.6 ± 11 | |||
| Cycling to work | ||||
| No | 101.8 ± 13.7 | 0.098 | ||
| Yes | 99.8 ± 14.4 | |||
| Family H/O kidney disease | ||||
| No | 100.3 ± 14.2 | 0.269 | ||
| Yes | 104.2 ± 12.5 | |||
| Body mass index | ||||
| Underweight | 103.1 ± 17.4 | 0.448 | ||
| Normal range | 101.7 ± 14.5 | |||
| Overweight | 99.6 ± 12.3 | |||
| Obese | 99.9 ± 14.7 | |||
| Abdominal obesity | ||||
| No | 99.7 ± 15.4 | 0.316 | ||
| Yes | 100.8 ± 13.3 | |||
| HSSI category | ||||
| Green zone | 100.9 ± 14.5 | 0.762 | ||
| Yellow zone | 100.4 ± 15.5 | |||
| Red zone | 100 ± 13.3 | |||
| Nonvisible hematuria | ||||
| No | 100.4 ± 13.9 | 0.884 | ||
| Yes | 100 ± 20.4 | |||
| Proteinuria | ||||
| No | 100.5 ± 14.2 | 0.158 | ||
| Yes | 94.4 ± 14.8 | |||
HSSI: Heat strain score index, H/O: History of.
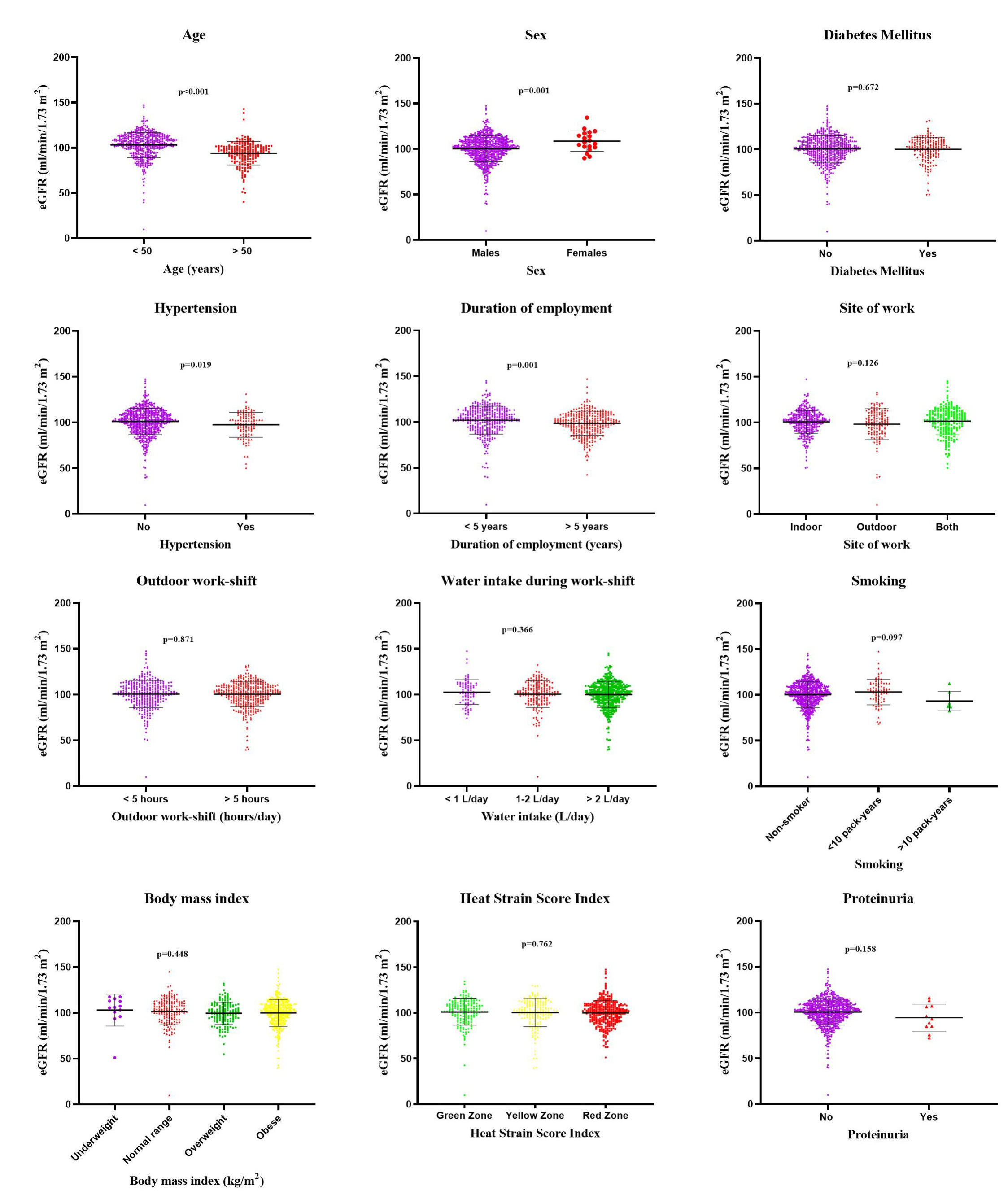
- Factors affecting glomerular filtration rate of security personnel. eGFR: Estimated glomerular filtration rate.
Follow-up
Anti-hypertensive medications were started in 40/49 newly detected hypertensives and treatment modifications were made in 10/59 known hypertensives. Oral anti-diabetic agents were started in 62/83 newly detected diabetics and dose adjustments were made in 15/90 known diabetics. Insulin was started in six newly detected and five known diabetics. In addition to dietary and life-style modifications, anti-obesity drugs were prescribed to five officers. Nutritional anemia was treated with oral iron (21/27), vitamin B12 (4/27), and folic acid (2/27) supplements.
Nine of twenty participants with “probable CKD” were diagnosed to have “definite CKD” on repeat testing after 3 months. Three out of nine had diabetes, 2/9 had hypertension, and proteinuria was <0.5 g/day in all of them. Six participants (0.9%) met diagnostic criteria of CKDu. Renin angiotensin system blockers were initiated in all nine patients. Net clinical benefit (initiation, modification, or change in medication) was seen in 170/678 (25.1%) participants.
Discussion
Security officers in hot tropical countries form a unique occupational cohort as their job pattern exposes them to a sedentary lifestyle and heat stress. We observed a high prevalence of obesity (50.4%), diabetes (25.5%), and hypertension (15.9%) in our cohort. Data from National Health Interview Survey 2010 reported that 27.7% of US workers were obese. Among occupational categories, protective service workers had the highest incidence of obesity (40.7%).21 In a cross-sectional study of 963 security personnel working in six private security organizations at Istanbul, prevalence of overweight, obesity, and morbid obesity were 57, 14.4, and 0.4% respectively.22 Possible causes for such a high burden of noncommunicable diseases are long periods of physical inactivity, irregular diet and limited choice of food on duty, disrupted sleep and stress due to overtime and shift work, and high rates of alcohol and tobacco consumption as compared to the general population.23,24
Almost half of our cohort had definite heat stress in the red zone. Similar findings have been reported in other occupational sectors in India using different heat stress indices. In a study of 442 workers from organized and nonorganized workplaces in South India, 82 and 42% were exposed to higher than recommended threshold limit values (TLVs) in summer and winter, respectively. Workers with heavy workload were exposed to higher occupational heat stress, had more heat-related health issues, and reduced productivity.18 Wet bulb globe temperature (WBGT) measurements (environmental heat strain index) were made over a 4-year period at 100 locations of automotive manufacturing units in Chennai. Measurements were made during the hottest part of the day (11am–2.30 pm) and month (May or June). Twenty-eight percent of workers had TLV above the recommended range.19
Heat stress was found to be higher in those working outdoors and with longer duration of employment in our cohort. Similar findings were observed in a cross-sectional study of 35 diesel power plant operators in an Indonesian state electricity company wherein heat stress assessed by HSSI was found to be higher in older workers, those with longer employment duration, and with poor hydration status.25 In the Thai cohort study, heat stress assessed in 37,816 full-time workers with a questionnaire was found to be higher in men, those with lower education and income, those involved in physical jobs as compared to office work, workers in rural areas, and regular drinkers and smokers.26 Cumulative heat exposure with longer employment duration and decrease in functional sweat glands in older individuals altering sweat rates may be the possible causes.27 HSSI scores did not differ between men and women in our cohort. In a study of 261 outdoor workers in Anuradhapura district of Sri Lanka, heat stress scores were found to be higher in women. The authors postulated that even though women have a higher density of activated sweat glands as compared to men, sweat rate is lower, leading to higher core temperatures.28 However, women security officers in our cohort were younger and thus having lower cumulative heat exposures. Interestingly, HSSI scores in our cohort were not affected by BMI, but those with abdominal obesity had lower scores. Theoretically, body fat has low conductivity which results in low passage of heat from surface to blood.29 However, clinical trials have shown conflicting results on the effect of obesity on heat strain.30,31 Obese individuals produce less physical work and this might have led to lower HSSI scores in officers with abdominal obesity in our cohort.
In our study, we observed that the eGFR was lower in older officers, those with longer employment duration, those who had hypertension, and those who were smokers. Hypertension is a risk factor for both development as well as rapid progression of CKD. Also, decline in eGFR can cause hypertension due to volume expansion and increase in systemic vascular resistance.32 This temporality of exposure and outcome cannot be ascertained with confidence in a cross-sectional study. The effect of smoking on eGFR is controversial with studies showing active smokers have a higher,33,34 lower,35 or no difference36 in eGFR as compared to nonsmokers.
In our cohort of security officers, we did not find any correlation between HSSI scores and eGFR. The concept of heat stress nephropathy was first described among sugarcane workers in Central America and was known as “Mesoamerican Nephropathy.”37 Sugarcane harvesting is done over a period of 5 months (known as “zafra”) and involves 4–12 hours of intense labor in temperatures of 34–42°C.38 Physical exertion in heat causes reduction in renal blood flow which reduces oxygen delivery to renal tubules causing depletion of adenosine triphosphate (ATP) leading to acute tubular injury.39 Repeated episodes of AKI can then progress to CKD.
The job profile of security officers, however, does not involve intense physical activity. The other important determinant of heat stress nephropathy is chronic dehydration. Prolonged periods of dehydration cause an increase in osmolality leading to vasopressin secretion which increases urinary concentration. Chronic dehydration also causes renal vasoconstriction and decrease in eGFR. In a study carried out at a sugar mill in Nicaragua during 2017–2018 (“harvest period 1”), Glaser et al. noted that workers involved in most strenuous work (burned cane cutters) had a greater decline in cross-harvest eGFR as compared to those carrying out less strenuous work (seed cutters, irrigation repair workers, and field support staff). Interventions like hydration, cooling techniques, and regulation of work were introduced during “harvest period 2” (2018–2019). Cross-harvest eGFR-decline and AKI rates in burned cane cutters were lower during “harvest period 2.”40,41 Acidic urine, a marker of intravascular dehydration was more common in those working outdoors and consuming <2 L of water during the 8-hour work shift in our study.42 The impact of heat stress did not translate into the kidney function of our security officers probably due to lack of strenuous physical activity and good hydration habits observed in the majority of our cohort.
To the best of our knowledge, this is the first study looking into factors affecting eGFR in a large cohort of security officers. The strengths of our study are the large size of our cohort, CKD being defined as per KDIGO definition, use of validated questionnaires adapted to local population, and clinical impact of the program in treatment modifications. Our study, however, is not without limitations. We used HSSI which is an observational-perceptual tool to assess heat stress. Environmental and physiological indices were not used due to cost and invasive nature of the tests.43 Being a cross-sectional study, a causal inference cannot be made due to problems of reverse causality and survivorship bias, which would need future longitudinal studies. Our institute follows occupational guidelines for heat-related preventive measures rigorously which could impact the outcomes of our study. This is evident in majority having good hydration habits. However, in spite of all these measures, almost half of the cohort had heat stress in the red zone.
We observed a high prevalence of obesity, diabetes, and hypertension in security personnel working at our tertiary care center. Almost half of the cohort had definite heat stress. Heat stress was higher in those working outdoors and with longer employment duration and lower in those with abdominal obesity. eGFR was lower in older officers, smokers, hypertensives, and those with longer employment duration. Less than 1% of officers developed CKDu. eGFR was unaffected by the high levels of heat stress observed in security officers. Future longitudinal occupational cohort studies are needed to understand the pathomechanisms of differential impact of heat stress on kidney function of agricultural and nonagricultural workers.
Acknowledgements
We would like to thank Mr. W. Abdul Latheef (Chief Security Officer), Mrs. Vimala S. (Laboratory Auxiliary Instructor), Mr. Santhosh Kumar R. and Merci Nahomi Deborah (translators), and Mr. P. Gowri Shankar (research coordinator). We would like to thank all the nurses, dialysis technicians, students, dieticians, and physicians for their wholehearted dedication in running this program.
Financial support and sponsorship
The work was supported by the Internal major grant no: 12003 to EEJ dated 24.04.2019 from Christian Medical College Vellore.
Conflicts of interest
There are no conflicts of interest.
References
- Metabolic syndrome and other cardiovascular risk factors among police officers. N Am J Med Sci. 2012;4:630-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence and risk factors of hypertension among male police personnel in urban Puducherry, India. Kathmandu University Medical Journal. 2015;12:242-6.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of obesity and it’s associated risk factors among policemen of Chitradurga district, Karnataka, India. Int J Adv Med. 2018;5:1280.
- [CrossRef] [Google Scholar]
- Impacts of climate change and heat stress on farmworkers’ health: A scoping review. Front Public Health. 2022;10:782811.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Occupational heat exposure alone does not explain chronic kidney disease of uncertain aetiology (CKDu) in Sri Lanka. The Journal of Climate Change and Health. 2022;8:100143.
- [CrossRef] [Google Scholar]
- Heat and PAHs emissions in indoor kitchen air and its impact on kidney dysfunctions among kitchen workers in Lucknow, North India. PLoS One. 2016;11:e0148641.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A comparison and appraisal of a comprehensive range of human thermal climate indices. Int J Biometeorol. 2017;61:487-512.
- [CrossRef] [PubMed] [Google Scholar]
- Development and validation of a questionnaire for preliminary assessment of heat stress at workplace. J Res Health Sci. 2015;15:175-81.
- [PubMed] [Google Scholar]
- Validation of a questionnaire for heat strain evaluation in women workers. Int J Prev Med. 2013;4:631-40.
- [PubMed] [PubMed Central] [Google Scholar]
- Construct validation of a heat strain score index with structural equation modeling. Health Serv Res. 2011;6:601-12.
- [Google Scholar]
- Investigation of thermal exposure in traditional neyshabur bakeries using heat strain and physiological indices. MethodsX. 2019;6:355-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Heat stress level and physiological parameters among an open-pit mine workers in Razavi Khorasan, Iran. Ann Med Health Sci Res. 2017;7
- [Google Scholar]
- Translation and validation of study instruments for cross-cultural research. Gastroenterology. 2004;126:S124-S8.
- [CrossRef] [PubMed] [Google Scholar]
- First morning voids are more Reliable than spot urine samples to assess microalbuminuria. J Am Soc Nephrol. 2009;20:436-43.
- [CrossRef] [PubMed] [Google Scholar]
- The world health organization stepwise approach to noncommunicable disease risk-factor surveillance: Methods, challenges, and opportunities. Am J Public Health. 2016;106:74-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Classification and diagnosis of diabetes: Standards of medical care in diabetes-2022. Diabetes Care. 2022;45:S17-S38.
- [CrossRef] [PubMed] [Google Scholar]
- Hypertension update, JNC8 and beyond. Curr Opin Pharmacol. 2017;33:41-6.
- [CrossRef] [PubMed] [Google Scholar]
- Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for asian indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009;57:163-70.
- [PubMed] [Google Scholar]
- Estimating GFR using the CKD epidemiology collaboration (CKD-EPI) creatinine equation: More accurate GFR estimates, lower CKD prevalence estimates, and better risk predictions. Am J Kidney Dis. 2010;55:622-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Epidemiology of chronic kidney disease: An update 2022. Kidney Int Suppl. 2022;12:7-11.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of obesity by occupation among US workers. J Occup Environ Med. 2014;56:516-28.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Investigation of nutritional status of security officers working in shifts and correlation with obesity: Evaluation of nutritional status of security officers working in shifts. Progress in Nutrition. 2019;21:276-84.
- [Google Scholar]
- Shiftworking, Nutrition and Obesity: Implications for workforce health-a systematic review. Asia Pac J Clin Nutr. 2013;22:505-15.
- [CrossRef] [PubMed] [Google Scholar]
- The Factors influencing the eating behaviour of shiftworkers: What, when, where and why. Ind Health. 2019;57:419-53.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Heat strains among diesel power plant operators and related factors. Indian J Public Health Res Dev. 2020;11:1262-7.
- [Google Scholar]
- Risk of chronic kidney disease in patients with heat injury: A nationwide longitudinal cohort study in Taiwan. PLoS One. 2020;15:e0235607.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Aging-related shift of eccrine sweat glands toward the skin surface due to tangling and rotation of the secretory ducts revealed by digital 3d skin reconstruction. Skin Res Technol. 2021;27:569-75.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Relevance of heat stress and dehydration to chronic kidney disease (CKDu) in Sri Lanka. Prev Med Rep. 2019;15:100928.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Adipose tissue as an endocrine organ. J Clin Endocrinol Metab. 2004;89:2548-56.
- [CrossRef] [PubMed] [Google Scholar]
- Relevance of individual characteristics for human heat stress response is dependent on exercise intensity and climate type. Eur J Appl Physiol Occup Physiol. 1998;77:231-41.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of obesity on body temperature in otherwise-healthy females when controlling hydration and heat production during exercise in the heat. Eur J Appl Physiol. 2015;115:167-76.
- [CrossRef] [PubMed] [Google Scholar]
- A Feared Combination: Hypertension and chronic kidney disease. J Clin Hypertens. 2019;21:102-4.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The differential effect of cigarette smoking on glomerular filtration rate and proteinuria in an apparently healthy population. Hypertens Res. 2009;32:214-9.
- [CrossRef] [PubMed] [Google Scholar]
- Alcohol and cigarette consumption, renal function and blood pressure in middle-aged healthy men. J Hum Hypertens. 2007;21:966-8.
- [CrossRef] [PubMed] [Google Scholar]
- The association among smoking, heavy drinking, and chronic kidney disease. Am J Epidemiol. 2006;164:263-71.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and factors associated with CKD: A population study from beijing. Am J Kidney Dis. 2008;51:373-84.
- [CrossRef] [PubMed] [Google Scholar]
- Climatological nephropathy: An overview. Int J Health sci Res. 2021;11:83-96.
- [CrossRef] [Google Scholar]
- Decline in kidney function among apparently healthy young adults at risk of mesoamerican nephropathy. J Am Soc Nephrol. 2018;29:2200-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical evidence of acute mesoamerican nephropathy. Am J Trop Med Hyg. 2017;97:1247-56.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Preventing kidney injury among sugarcane workers: Promising evidence from enhanced workplace interventions. Occup Environ Med. 2020;77:527-34.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Workload and cross-harvest kidney injury in a nicaraguan sugarcane worker cohort. Occup Environ Med. 2019;76:818-26.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Correlation of pH in urine with capacity of drinking water per Day. Int J Res Stud Microbiol Biotechnol. 2019;5:2454-9428.
- [CrossRef] [Google Scholar]
- challenges in conducting epidemiological field studies evaluating associations between heat stress and renal health among workers in informal sectors: Experiences from India. Environ Res. 2021;200:111343.
- [CrossRef] [PubMed] [Google Scholar]







