Translate this page into:
Impact of the Lockdown on Patients Receiving Maintenance Hemodialysis at a Tertiary Care Facility in Southern India – A Mixed-methods Approach
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aims:
The mass quarantine measures adopted to control the COVID-19 pandemic greatly impacted the lives of patients on haemodialysis in India. We used a mixed methods approach to study its effect on dialysis outcomes and the lived experience of haemodialysis patients during the lockdown.
Methods:
Quantitative data was collected from 141 subjects using a structured proforma to determine the impact of the lockdown on dialysis outcomes and travel expenses. Qualitative data collected through in-depth interviews with 9 patients by purposive sampling were recorded and transcribed to explore the lived experience of haemodialysis patients during lockdown. The cohort was followed up till October 31st 2020 for incidence of COVID-19, deaths, and dropouts.
Results:
The median increase in per day travel expense was 25%. Due to decrease in dialysis frequency, patients previously on thrice weekly haemodialysis experienced significant increase in pre-dialysis systolic blood pressure (P = 0.005) compared to those on twice weekly haemodialysis. Between March 25th and July 15th 2020, 12 patients (8.5%) required emergency dialysis sessions, and 4 patients (2.8%) required admissions for hypertensive emergencies. Four main themes emerged from thematic analysis of transcribed interviews: Travel inconveniences, uncertainty resulting in anxiety, financial burden and frequency change in dialysis leading to worsening of symptoms. Twenty-two patients (15.6%) were diagnosed with COVID-19, the first case diagnosed 33 days after the first ‘unlock’ phase.
Conclusion:
The lockdown was successful in delaying infection transmission but had unintended physical and psychosocial effects on haemodialysis patients.
Keywords
COVID-19
hemodialysis
India
lockdown
outcome measures
Introduction
On March 24, 2020, in response to a surge in the number of COVID-19 infections, the Government of India announced a nationwide lockdown, halting all but essential services. Published data from India has focused on the impact of the lockdown from the provider perspective, namely, missed dialysis sessions, dropouts from dialysis, requirement for emergency dialysis sessions, and death.[1] In contrast, there is no data on how the lockdown affected individual patients and their families. This study used a mixed-methods approach to provide a comprehensive overview of the impact of the lockdown on the experience and dialysis outcomes of patients on maintenance hemodialysis (HD).
Methods
The study was conducted in the dialysis unit of a large private, not-for-profit, tertiary care facility in southern India that caters to over 200 prevalent HD patients. All patients on thrice-weekly HD (3wHD) were shifted to a twice-weekly schedule (2wHD) after the lockdown was imposed.
Study design and participants
From April 8 to 30, 2020, consecutive prevalent HD patients who had been on dialysis for at least 3 months prior to the imposition of the lockdown were recruited. Investigators used a structured proforma to collect demographic, socioeconomic, and clinical information from dialysis records and face-to-face interviews conducted at the dialysis unit in the participants’ native language. To study the impact of a decrease in HD frequency to twice a week, interdialytic weight gain and predialysis blood pressure 2 weeks preceding and following the lockdown, and laboratory investigations (hemoglobin, serum sodium, potassium, bicarbonate, calcium, and phosphate), within 1 month before and after the lockdown, were compared. Data on emergency dialysis sessions and emergency department or in-patient admissions attributable to volume overload was collected till July 15, 2020, at which point schedules were revised back to their pre-lockdown status. Participants were followed up from study recruitment till October 31, 2020 (when the last lockdown restrictions were lifted across the country) or their last HD session at our institution (whichever was earlier) for incidence of COVID-19, dropouts, and deaths. COVID-19 infection was defined as nasopharyngeal swab positive for SARS COV-2 with or without symptoms. Severity was classified based on the WHO ordinal severity scale.
A descriptive qualitative design was used to explore the experience of a group of patients undergoing maintenance HD during the lockdown. Purposive sampling was used to select nine patients from among those already recruited in the study who represented different age groups, gender, dialysis duration, and geographical locations to obtain a diverse range of experiences. Data was collected through semi-structured, in-person, in-depth interviews conducted in the dialysis unit at a time convenient for participants, in their native language. The sample size was determined by data saturation. Expedited ethics approval for this research was received from the institutional review board. Written informed consent was obtained before data collection for the quantitative and qualitative components of the study.
Data analysis
Quantitative data collected was computed and analyzed using measures of central tendency and the paired t-test or Wilcoxon signed-rank test as applicable. The details of qualitative data analysis are given in the supplementary material.
Results
Figure 1 gives the STROBE diagram for this study. The mean age of the participants was 51 years, 66% were males, 60% were on 3wHD prior to the lockdown, and 73% paid for dialysis out of their own pocket [Table 1]. Patients on 3wHD and 2wHD did not differ in these baseline characteristics (analysis not shown).

- STROBE diagram for the study
| Mean±SD, median (IQR), or percentage | |
|---|---|
| Age (years) | 51.2±15.2 |
| Males (%) | 66.7 |
| Diabetes (%) | 44 |
| Median Charlson’s comorbidity index (IQR) | 4 (2, 6) |
| Median dialysis vintage (months, IQR) | 20 (9.7, 53) |
| On thrice-weekly hemodialysis (%) | 60.3 |
| Native kidney disease (%) | 41.1 |
| Diabetic nephropathy | 31.2 |
| Unknown Glomerular | 14.2 |
| Hypertensive nephrosclerosis | 4.3 |
| Inherited kidney disease | 3.5 |
| Urological disease and CAKUT | 4.3 |
| Interstitial disease | 1.4 |
| Dialysis financed by (%) | |
| Self | 73.6 |
| Employer (private/government) | 21.4 |
| Insurance | 5.0 |
| Education (%) | |
| No formal schooling | 4.3 |
| Primary school | 7.8 |
| Middle school | 15.6 |
| High school | 30.5 |
| Undergraduate | 27.0 |
| Postgraduate | 9.9 |
| Professional | 5.0 |
| Occupation (%) | |
| Unemployed but able to work | 11.3 |
| Unemployed and unable to work | 10.6 |
| Private sector | 11.3 |
| Government sector | 15.6 |
| Self-employed | 12.8 |
| Homemaker | 20.6 |
| Student | 4.3 |
| Retired | 13.5 |
| Median distance between home and | 8 (3, 32) |
| dialysis unit (km, IQR) | Range: 0.5-150 km |
CAKUT: Congenital anomalies of the kidney and urinary tract
Following the imposition of the lockdown, the proportion of patients availing of autorickshaws, taxis, and public transport declined from 73 to 17% [Table 2], in favor of private vehicles (68%). The number of patients who travelled on foot quadrupled. While the time taken to reach the dialysis unit remained unchanged, there was a median 25% increase in daily transport costs from pre-lockdown values.
| Before the lockdown (% or median, IQR) | During the lockdown (% or median, IQR) | P | |
|---|---|---|---|
| Mode of transport to the dialysis unit (%) | <0.001 | ||
| Private vehicle | 23.4 | 68.8 | |
| Autorickshaw/taxi | 39.7 | 17.7 | |
| Public transport (bus/train) | 33.3 | 0 | |
| On foot | 3.6 | 12.1 | |
| Ambulance | 0 | 1.4 | |
| Median time taken to travel to the dialysis unit (hours) | 0.5 (0.25, 1) | 0.5 (0.25, 1) | 0.307 |
| Median per day expense on transport to the dialysis unit (rupees) | 150 (50, 250) | 200 (80, 500) | <0.001 |
| Median increase over usual expense (%) | 25 (0, 172) |
When patients who were on 3wHD and 2wHD schedules before the lockdown were compared [Table 3], both groups showed significant increases in median IDWG (+0.5 kg vs. +0.25 kg, P = 0.423 between groups) and a decrease in median serum sodium (-1 vs. -2 meq/L, P = 0.527 between groups) from pre-lockdown values, in the month following the lockdown. The 3wHD group also experienced an increase in median predialysis systolic blood pressure (+10 mm Hg, vs. 0 mm Hg, P = 0.005 between groups) and diastolic blood pressure (+2 mm Hg, vs. 0 mm Hg, P = 0.062 between groups). The 2wHD group experienced an increase in serum bicarbonate (+1 meq/L vs. – 1 meq/L, P = 0.091 between groups) and a decrease in serum phosphate (- 0.5 mg/dL vs. 0 mg/dL, P = 0.263 between groups). In a subset of this cohort who were on the same dialysis frequency in 2019 (n = 49), serum sodium was found to decrease significantly in both 2wHD and 3wHD patients, with no difference between groups, and was comparable between 2019 and 2020 [P = 0.948, Supplementary Table 1].
| Patients previously on thrice weekly Dialysis (Median, IQR) | P§ | Patients previously on twice-weekly Dialysis (Median, IQR) | P§ | P between groups | |
|---|---|---|---|---|---|
| Median change in predialysis systolic blood pressure in mm Hg (IQR)† n=141 | +10 (20) | <0.001* | 0 (10) | 0.235 | 0.005* |
| Median change in predialysis diastolic blood pressure in mm Hg (IQR)† n=141 | +2 (10) | 0.016* | 0 (0) | 0.929 | 0.062 |
| Median change in interdialytic weight gain in kg (IQR)† n=141 | +0.5 (0.9) | <0.001* | +0.25 (1.1) | 0.045* | 0.423 |
| Median change in hemoglobin in g/dL (IQR) †† n=128 | +0.05 (2.4) | 0.759 | +0.35 (2.0) | 0.597 | 0.864 |
| Median change in serum sodium in meq/L†† n=128 | - 1.0 (4.5) | 0.013* | - 2.0 (5.0) | 0.007* | 0.527 |
| Median change in serum potassium in meq/L †† n=130 | +0.15 (1.3) | 0.063 | +0.05 (1.4) | 0.576 | 0.522 |
| Median change in serum bicarbonate in meq/L †† n=128 | -1.0 (6.0) | 0.985 | +1.0 (7.0) | 0.037* | 0.091 |
| Median change in serum calcium in mg/dL†† n=107 | +0.04 (0.8) | 0.136 | +0.1 (0.8) | 0.102 | 0.750 |
| Median change in serum phosphate in mg/dL†† n=108 | 0 (1.9) | 0.725 | -0.5 (1.45) | 0.047* | 0.263 |
† Average of consecutive values obtained 2 weeks before and after lockdown was imposed. †† Comparison between tests done within 1 month before and after lockdown was imposed. §P value for intragroup change in parameter before and after lockdown
| Patients on thrice-weekly Dialysis (Median, IQR) | P§ | Patients on twice-weekly dialysis (Median, IQR) | P§ | P between groups | |
|---|---|---|---|---|---|
| Median change in hemoglobin in g/dL (IQR)† | +0.03 (1.4) | 0.135 | +0.1 (1.6) | 0.899 | 0.207 |
| Median change in serum sodium in meq/L† | -1.0 (4.0) | 0.027* | -1 (5.0) | 0.003* | 0.901 |
| Median change in serum potassium in meq/L† | +0.2 (0.75) | 0.126 | -0.2 (0.8) | 0.588 | 0.135 |
| Median change in serum bicarbonate in meq/L† | -1.5 (5.5) | 0.117 | 0 (5) | 0.613 | 0.490 |
| Median change in serum calcium in mg/dL† | -0.05 (0.58) | 0.241 | -0.1 (0.6) | 0.174 | 0.964 |
| Median change in serum phosphate in mg/dL† | 0.3 (1.58) | 0.404 | 0 (1.6) | 0.193 | 0.594 |
† Comparison between tests done in March 2019 and April 2019. § P value for intragroup change in parameter. Note: Data for interdialytic weight gain and predialysis systolic and diastolic blood pressure was not available for this time period
Between March 25 and July 15, 2020, 12 patients (8.5%) required 14 emergency dialysis sessions for fluid overload compared to four patients (8.1%) in 2019 (P = 0.93), and 4 patients (2.8%) had emergency department or ward admissions for pulmonary edema or hypertensive emergencies, compared to none, in 2019 (P = 0.23). Till October 31, 2020, 22 patients (15.6%) were diagnosed with COVID-19: Asymptomatic COVID19 (n = 5), WHO ordinal scale 3 (n = 9), Scale 4 (n = 3), Scale 5 (n = 2), and Scale 7 (n = 3). The first case was diagnosed on July 4, 2020, approximately 1 month after the first “Unlock” phase was announced [June 1, 2020, Figure 2]. There were seven dropouts (4.9%) and eight deaths (5.6%); the causes being COVID19 (n = 2), sepsis (n = 2), hypertensive emergency (n = 1), and sudden death at home (n = 3).
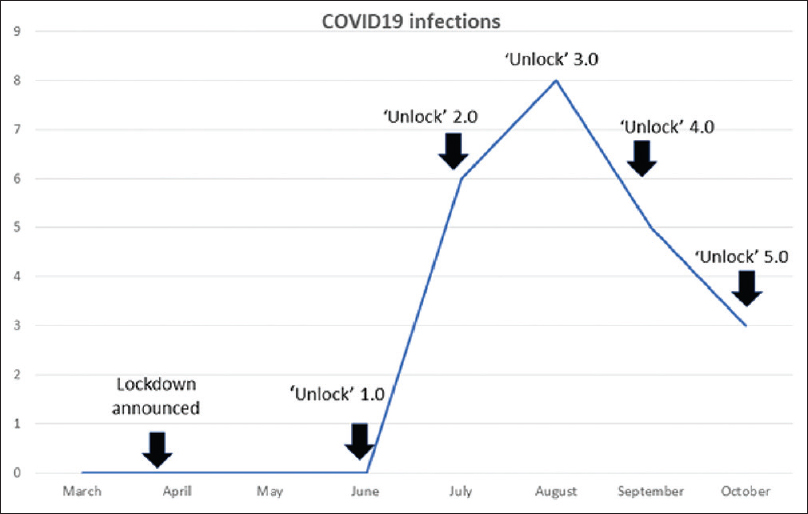
- Temporal association of various phases of the lockdown with COVID-19 infection incidence in the cohort
Qualitative data
Thematic redundancy was achieved with the ninth interview; hence, the sample size was 9.
The themes that emerged from the analysis of the interviews can be categorized as (TUFF):
-
Travel inconveniences
-
Uncertainty resulting in anxiety
-
Financial burden
-
Frequency change in dialysis leading to worsening of symptoms
1.Travel inconveniences
“My house is just 2 kilometres away from hospital. Since the lockdown, getting an auto to come to the hospital was difficult. Many days I came by walk, but going back after dialysis by walk in the hot sun was very tiring. When an auto was willing to come, they demanded extra fare.” (P2)
“I come from T, a place 100 kms away from hospital. Before the lockdown, me and my husband took public transport (bus) and the expense was only 250 to 300 rupees. Now with the lockdown, we are coming in the car of a known person. We had to pay for the driver and petrol. The petrol charges alone came to 850 rupees.” (P7)
2.Uncertainty resulting in anxiety
“I had been on treatment at this facility for my kidney disease for 2 yrs. I am a medical student, doing internship. We reached here from Sikkim in January wanting to get a renal transplant, expecting that workup would be over by March. But the process got delayed due to the lockdown. My uncle also is here ……… he's stuck here with us, leaving his wife and children. Couldn’t go back because of lock down.” (P2)
“My transplant planning was going on when the lockdown was declared. The expenses of living outside and having to come for dialysis twice a week is more. I cannot be without treatment, at the same time cannot have the treatment also!!” (P5)
When asked whether they were anxious about getting COVID due to their decreased immunity, most said they were taking adequate precautions but were worried about having to come to the hospital twice a week.
Forty-seven-year-old P3 who is living alone with her elderly father said, “I strictly follow wearing of mask and social distancing. I was most worried about whether I’ll become sick or breathless in the night. What will my father do? How will he bring me to the hospital? I should not be a burden for him.”
“I am not going out of the house except to come to the hospital. On the days that I come to hospital I’m very scared about meeting many people and getting the virus” (P3).
3.Financial burden
“Had to spend around 5 lakh (500,000) rupees till now. I’m not from a rich family. We are poor and had prepared for kidney transplant with much difficulty. Having to undergo dialysis for another 6 months increased my expense and I had to use up the money kept for transplant. It's necessary and I cannot avoid the expense, but there are problems. I’ll see what I can do.” (P6)
“I spend 70,000 rupees every month on travel, living expenses and dialysis.” When asked about where he stayed, he said: “Seven of us are staying in this small place- one room, one small dining space and a kitchen.” (P8)
“I took leave from my job for kidney transplant and now I’m stuck here …. have to get dialysis three times a week ……. not sure whether I’ll be able to continue in the job. My wife who's working as teacher in a private school is getting only half pay due to lockdown. My parents are supporting us financially. We’re very much affected……. I also need to get costly injections to maintain my Hb…. It is very difficult!!” (P9)
4.Frequency change in dialysis leading to worsening of symptoms
“I did not have any breathing difficulty, tiredness or problem eating food. But the difficulty was in restricting water intake. I used to drink more water when I was getting thrice weekly dialysis. With two dialysis sessions I reduced my water intake to half which was very difficult!!(P8)
“I was advised to have 3 dialysis per week as I was waiting for transplant, then due to lockdown it was reduced to twice a week. It was hard… It's very hot… I want to drink more water, but I have to control because I am coming for dialysis only twice a week. It was very difficult to manage. I could not take food well, I became breathless, developed swelling of legs also…” (P9)
“Weight gain between dialysis sessions was always less than 1 kg for me, but I felt that nausea increased and my food intake decreased.’ (P2)
An unexpected finding was that some of the participants were happier with twice-weekly dialysis, reporting that they did not experience any increase in severity of symptoms on receiving two sessions a week.
“On receiving 3 dialysis a week, I used to be more tired. With 2 dialysis, I am feeling good except that there is more weight gain between dialysis sessions. I am able to eat everything, no nausea or vomiting and no swelling on the legs or breathlessness between dialysis sessions. I only go out and buy things required for the house” (P1)
Resilience and a stoic spirit were also evident in all the participants, as they accepted the situation as “inevitable” and hoped for a return to normalcy.
Discussion
The lockdown was announced just as the country was heading into a typically hot and humid summer. As patients struggled to regulate their fluid intake, our findings show that the decrease in HD frequency resulted in an increase in predialysis blood pressures and IDWG, especially among patients who were previously on a 3wHD schedule. Although we did not collect data on residual kidney function, this is likely to have been significantly different between the 3wHD and 2wHD groups,[2] apart from 3wHD patients being “habituated” to a more liberal fluid intake, as hinted by P8 in one of the highlighted excerpts. This had serious consequences: increased requirement for outpatient emergency HD, in-patient admissions, and at least one death directly attributable to fluid overload, though not significantly different from 2019.
Serum sodium decreased in the 3wHD and 2wHD groups, likely due to an increase in interdialytic weight gain, though this difference was no different from that seen in 2019. The increase in serum bicarbonate and decrease in serum phosphate in the 2wHD group who remained on an unchanged schedule (not seen in 2019) is intriguing, any may be due to reduced quantum and quality of protein intake. Although we did not collect information on how the lockdown affected dietary habits or family income, the 2wHD cohort is largely composed of the economically deprived sections, the majority of whom work in the informal sector without a secure income and may have been disproportionately affected by the economic repercussions of the lockdown.[3] The interviews also shed light on the subtle symptoms of underdialysis patients experienced when dialysis frequency was reduced – nausea and loss of appetite (P2). This is consistent with reports of a lower normalized protein catabolic rate in patients on twice-weekly HD.[2]
Travel inconveniences – the limited availability of transport options and escalation in costs – were highlighted by patients. Transport expenditure affected patients across the board but was particularly harsh on those who were self-financed or lived far from the unit. Shuttle services to ferry patients to the unit may bring down transport expenses but has been shown to increase the risk of contracting COVID-19.[4] Travel vouchers linked to a mobile app that triangulates designated BLS-trained transport providers, patient movement, and attendance at the dialysis session[5] may be an option that provides financial relief while minimizing the risk of fraud. “Dialysis-on-wheels” to eliminate the need for patient transport may be an option in urban centers.[6]
Apart from the fear of contracting COVID19, suspension of elective transplant surgeries was a significant source of stress for outstation patients who were left stranded far from home. The financial implications of continuing dialysis are manifold: The average cost of an HD session varies from 1100 to 3500 rupees,[7] which is an out-of-pocket expenditure for the majority. Yet even in the few states where dialysis is funded via state-sponsored insurance schemes, only 53% remain on dialysis beyond 6 months because of the many indirect and hidden costs – transport, medications, management of complications and comorbidities, loss of income, and caregiver burden.[8] For patients awaiting transplant, dialysis eats into their savings, leaving them with little or no buffer to cushion the cost of transplant or posttransplant complications, should they arise. The lockdown also brought in its wake loss of job security and pay cuts (P9), which compounded patients’ financial woes.
In its main objective of reducing or delaying COVID-19 transmission, the lockdown appears to have been effective, as is clearly demonstrated by the temporal association between “unlocking” and a spike in infections in our cohort. The majority (78%) of infections had a severity of 4 or less on the WHO ordinal scale, while the two patients who succumbed had severe COVID-19 requiring intubation.
Conclusion
The lockdown resulted in travel inconveniences, uncertainty and anxiety, financial burden, and increased symptoms from decreased frequency of dialysis in HD patients but appears to have been successful in delaying transmission of COVID19 in this vulnerable population.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study was funded by an Internal Fluid Research Grant from our institution.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
This research was funded by an Institutional Fluid Research Grant from our institution. The authors wish to thank all patients who participated in this study – their strength and resilience in the face of insurmountable difficulties was an inspiration to us all. We hope that through these pages, their struggles will find a voice.
References
- The adverse effect of covid pandemic on the care of patients with kidney diseases in India. Kidney Int Rep. 2020;5:1545-50.
- [Google Scholar]
- Comparison of clinical outcome between twice- weekly and thrice-weekly hemodialysis in patients with residual kidney function? Medicine (Baltimore). 2016;95:e2767. doi: 10.1097/ MD.0000000000002767
- [Google Scholar]
- Implications of the COVID-19 pandemic for food security and social protection in India. Indian J Hum Dev. 2020;14:333-9.
- [Google Scholar]
- The keys to control a COVID-19 outbreak in a haemodialysis unit. Clin Kidney J. 2020;13:542-9.
- [Google Scholar]
- “Need a Ride.” improving transportation to dialysis treatment? J Nephrol Soc Work. 2016;40:28-42.
- [Google Scholar]
- Dialysis on Wheels. Available from: https://www. nephroplus.com/services/dialysis-on-wheels/
- Utilization, costs, and outcomes for patients receiving publicly funded hemodialysis in India. Kidney Int. 2018;94:440-5.
- [Google Scholar]
Supplementary Material
Qualitative data analysis
Interviews were conducted, transcribed, and analyzed by a female investigator (RRG). All audio recordings and transcripts were saved on a password-protected device. Confidentiality was ensured by using numbers instead of names (e.g., Participants – P1, P2) and removing identifying information from the transcripts. The audio recordings were transcribed to English manually by the investigator within 24 h of the interviews and were reviewed for accuracy. Throughout this study, we followed the Standards for Reporting Qualitative Research guidelines.
Each interview was transcribed verbatim, and thematic analysis was done to explore how people ascribe meaning to their experiences. Transcription, reading, and rereading transcripts further promoted familiarization with the data and helped in the generation of initial emerging themes. The transcripts were also analyzed in conjunction with the original recordings, so that the researcher became fully immersed in the data. The investigator then made an initial narrative summary of the key themes for an in-depth discussion with the wider team who independently analyzed the transcripts.
The credibility and transferability of data were ensured. Three investigators (RRG, VR, and ATV) analyzed the transcripts independently to gain the first-hand experience of the words of participants, allowing a richer interpretation. Findings were compared and discussed by the team for consensus on themes and theme categories. Variations of participant characteristics were considered, and sufficient quotations were collected through in-depth interviews to establish transferability. During the data analysis, the authors agreed with the results and chose the highlighted quotations.







