Translate this page into:
Mucormycosis of Autosomal Dominant Polycystic Kidney Disease
Corresponding author: Navaneethakrishnan Venkatachalam, Department of Urology, SRM Medical College Hospital and Research Centre, Mahatma Gandhi Road, Potheri, Chennai, Tamil Nadu, India. E-mail: drnavaneethakrishnan@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Venkatachalam N, Murugesan A. Mucormycosis of Autosomal Dominant Polycystic Kidney Disease. Indian J Nephrol. doi: 10.25259/IJN_373_2024
Abstract
Autosomal dominant polycystic kidney disease (ADPKD) is a relatively common indication for renal transplantation. Pre-transplant native nephrectomy in ADPKD needs to be individualized. We report a case of mucormycosis of ADPKD in an immunocompromised patient, which presents a novel clinical scenario for pre-transplant native nephrectomy.
Keywords
ADPKD
Native nephrectomy
Mucormycosis
Covid-19
Transplantation
Introduction
Autosomal dominant polycystic kidney disease (ADPKD) is the most common inherited renal cystic diseases and a common cause for pre-transplant native nephrectomy. Native nephrectomy carries significant morbidity, and the approach is tailored to individual needs.1 Mucormycosis is an opportunistic fulminant fungal infection. We report a case of mucormycosis of ADPKD in a young non-diabetic male with COVID-19 managed by pre-transplant native nephrectomy followed by renal transplantation.
Case Report
A 34-year-old, non-diabetic man with ADPKD on hemodialysis for 3 years presented with hematuria, acute urinary retention, and fever for 1 week. COVID-19 RTPCR was positive and CORADS score was 2. He was catheterized and quarantined. He had a previous episode of COVID-19 infection 6 months ago which he was managed with steroids for 1 week. Contrast CT abdomen showed bilateral enlarged polycystic kidneys with few hemorrhagic cysts on right lower pole [Figure 1]. Diagnostic cystoscopy and clot evacuation were performed. Lower tract was normal except for mild ooze from right ureteric orifice. Intractable hematuria warranted an open right native nephrectomy expediently as a damage control measure with COVID-19 safety precautions. Grossly, the kidney was enlarged and polycystic with a few hemorrhagic cysts. Microscopically, the significant finding was the presence of mucormycosis [Figure 2]. Intravenous Liposomal Amphotericin B was initiated. FDG PET CT showed no other active focus. COVID-19 RTPCR became negative after 2 weeks. Considering the possibility of occult disease in contralateral kidney and the risk of recurrence post-transplantation, he underwent open left native nephrectomy electively. The histopathology was negative for mucormycosis on the left. He was switched to oral posaconazole which was continued for 2 months. After 3 months, he underwent live allograft renal transplantation. He has been followed up for 2 years and remains well.
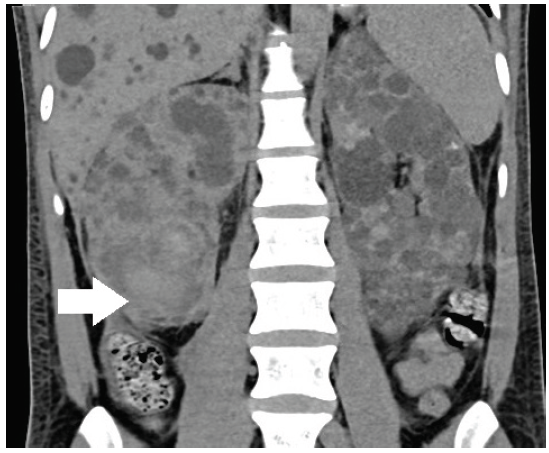
- Contrast CT of kidneys. Bilateral enlarged polycystic kidneys and liver. The hyperdense regions involving right lower pole (white arrow) indicate hemorrhagic cysts. CT: Computerized tomography.
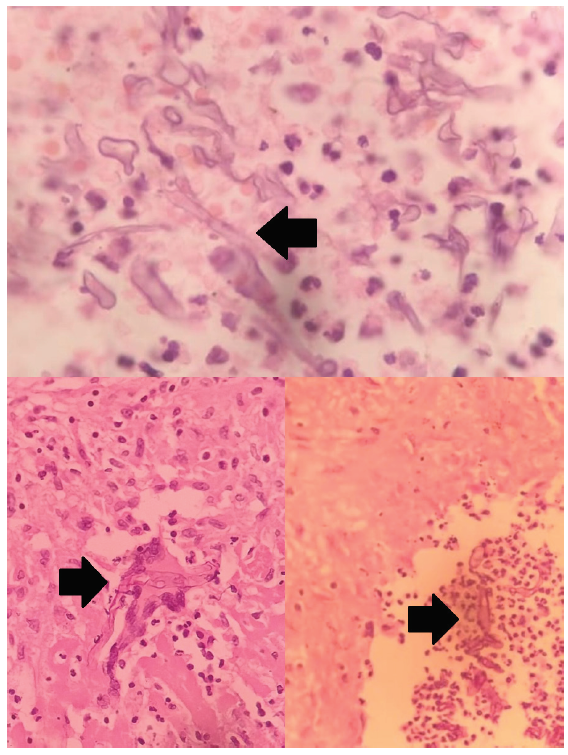
- Histopathology of right nephrectomy specimen. Broad aseptate hyphae with branching at right angle (black arrows) are consistent with mucormycosis.
Discussion
Although pyogenic infections are documented complications of ADPKD, the possibilities of fungal cyst infections are rare and opportunistic. Candidial infections are the commonest and can be successfully managed medically.2,3 Mucormycosis is a devastating fungal infection of particular interest after COVID-19 era. Immune dysregulation and corticosteroid misuse are the commonest cause for mucormycosis.4 Spores enter the cyst via bloodstream, from primary foci in respiratory or gastrointestinal tract via skin. Cyst infection manifest as a fairly confined disease unlike mucormycosis in a normal kidney which commonly occurs along with dissemination or rarely as isolated renal involvement and carries a dismal prognosis. Angioinvasion leads to spontaneous bleeding into the cyst causing loin pain or into the pelvicalyceal system causing hematuria. Blood culture is usually negative. Contrast CT localize the bleed but non-specific for mucormycosis. Diagnosis is often based on direct detection of fungal elements on histopathology and tissue culture. Conservative strategies such as medical therapy, angio-embolization, and percutaneous interventions are futile, time-consuming, and could potentially disseminate. Once diagnosed, FDG PET CT can be considered to exclude active focus elsewhere. Nephrectomy of the contralateral kidney was offered for the benefit of the doubt since the existence of dormant spores is possible asymptomatically, which cannot be excluded by other diagnostic modalities, and immunosuppression after renal transplantation could potentially lead to recurrence. Anti-fungal therapy after source control is recommended for 3 months.5,6
Conclusion
This is the first case report of mucormycosis of ADPKD. A high index of suspicion and early native nephrectomy pre-transplant led to a favorable outcome.
Acknowledgment
The authors acknowledge Department of Nephrology and Pathology for the photo courtesy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Tailoring the ‘perfect fit’ for renal transplant recipients with end-stage polycystic kidney disease: Indications and timing of native nephrectomy. In Vivo. 2017;31:307-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cyst infections in patients with autosomal dominant polycystic kidney disease. Clin J Am Soc Nephrol. 2009;4:1183-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Two cases of fungal cyst infection in ADPKD: Is this really a rare complication? BMC Infect Dis. 2019;19:911.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mucormycosis in COVID-19: A systematic review of case reported worldwide and in India. Diabetes Metab Syndr. 2021;15:102146.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Renal mucormycosis presenting during the COVID-19 pandemic: A series of 11 cases from a tertiary care center in India. Indian J Urol. 2022;38:115-20.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Potential role of 18F-FDG PET/CT in patients with fungal infections. AJR.. 2014;203:180-9.
- [CrossRef] [PubMed] [Google Scholar]







