Translate this page into:
Outcomes after Severe AKI Managed Outside ICU in Resource-Constrained Settings: A Prospective Cohort Study
*Onu Ugochi Chika and Prabhjot Kaur contributed equally to this work.
Corresponding author: Vivek Kumar, Department of Nephrology, Postgraduate Institute of Medical Education and Research, Chandigarh, India. E-mail: enigma165@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Chika OU, Kaur P, Singh N, Ramachandran R, Gupta KL, Kumar V. Outcomes after Severe AKI Managed Outside ICU in Resource-Constrained Settings: A Prospective Cohort Study. Indian J Nephrol. 2024;34:646-8. doi: 10.25259/ijn_168_23
Dear Editor,
Acute kidney injury (AKI) is common and associated with significant short-term as well as long-term morbidity and mortality. A meta-analysis on incidence of AKI and outcomes showed overall pooled incidence rates of AKI and AKI-associated mortality in adults as 21% and 23.3%, respectively.1 Globally, the incidence rates of AKI in hospitalized patients vary between 14.7% and 31.5%.1 A recent meta-analysis exploring the incidence of AKI in intensive care units (ICUs) in developed and developing countries reported similar incidence at 39.3% and 35.1%, respectively.2 The study highlighted the lack of data from developing countries and stressed the need for data from outside ICU settings.
Developing countries face higher burden of AKI with community-acquired AKI secondary to tropical infections, toxins, envenomations, and more being common.3,4 Access to timely medical care and dialysis are often suboptimal. Not all hospitalized patients with dialysis requiring AKI receive care in ICUs. At large tertiary care centers like ours, some patients with dialysis requiring AKI might continue to be cared for in waiting areas, emergency, general wards due to circumstantial compulsions. In the present prospective, observational, cohort study, we are reporting short-term outcomes at three months in patients with dialysis requiring Kidney Disease Improving Global Outcomes (KDIGO) stage 3 AKI, who were managed outside ICUs at our center in North India [Supplementary File 1].
Over three months between January and March 2017, 890 patients received hemodialysis at our center [Figure 1]. The participants received either hemodialysis or sustained low efficiency dialysis (SLED) if they were hemodynamically unstable. None received peritoneal dialysis or continuous renal replacement therapy (CRRT). Of these, 656 patients had AKI or AKI superimposed on chronic kidney disease (CKD). After excluding 452 patients, including those with known or suspected preexisting CKD, 204 were eligible for enrollment. However, 42 patients did not give consent and hence, 162 patients were enrolled. Average age was 49.4 ± 15.7 years with 67% being males [Table 1]. The median (interquartile range: IQR) duration of admission was nine (eight) days. Hypertension, diabetes mellitus, and heart disease were present in 36%, 36%, and 6% of patients, respectively. About 38% of patients did not report any preexisting disease or comorbidity. The most common causes of AKI were sepsis, decompensated liver disease, heart failure, pregnancy-related complications, and drug induced [Supplementary File 2 - Table S1]. Urinary tract and respiratory tract infections accounted for three-fourth of patients with sepsis related AKI. 74% of patients received care only in emergency areas and could not be moved to general wards or ICUs. Only four patients could be later shifted to ICUs after enrollment in the study.
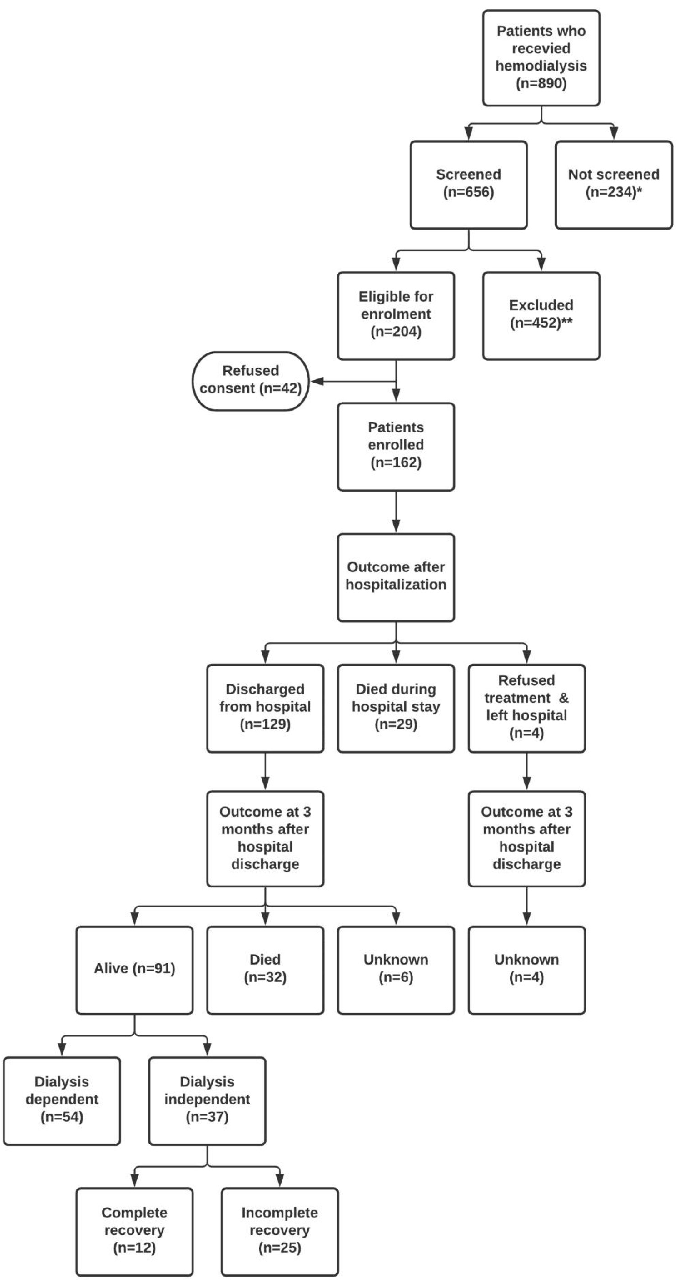
- Study enrolment, follow-up and outcomes. *Patients with end-stage kidney disease (ESKD) already on maintenance dialysis (n = 232), lithium intoxication (n = 2). **Preexisting pre-dialysis chronic kidney disease (n = 324), patients admitted to intensive care units (n = 56), solid organ transplant recipients (n = 8), history or presence of hepatitis C virus infection (n = 26), clinical diagnosis of glomerulonephritis (n = 17), history or presence of hepatitis B virus infection (n = 8), history or presence of human immunodeficiency virus infection (n = 2), and age <18 years (n = 11).
| Patient characteristics | At enrollment (n = 162) | At three-month follow-up (n = 91) |
|---|---|---|
| Age (years) | 49.43 ± 15.66 | 47.52 ± 15.50 |
| Gender (Male/Female) | 108/54 | 54/37 |
| S. creatinine (mg/dl) | 6.86 ± 3.85 | 4.31 ± 2.46 |
| S. urea (mg/dl) | 172.32 ± 90.20 | 95.10 ± 58.37 |
| Hemoglobin (g/dl) | 9.12 ± 2.63 | 10.26 ± 1.69 |
| S. total protein (g/dl) | 5.99 ± 1.32 | 6.66 ± 1.27 |
| S. albumin (g/dl) | 2.84 ± 2.44 | 3.05 ± 0.93 |
| S. uric acid (mg/dl) | 7.35 ± 2.50 | 5.77 ± 1.99 |
| S. total bilirubin (mg/dl) | 2.42 ± 5.72 | 1.49 ± 4.52 |
| S. conjugated bilirubin (mg/dl) | 1.16 ± 2.98 | 1.04 ± 2.98 |
| S. aspartate aminotransferase (U/L) | 33.50 (47.25) | 26.00 (17.00) |
| S. alanine aminotransferase (U/L) | 25.50 (54.00) | 21.50 (32.00) |
| S. alkaline phosphatase (U/L) | 147.00 (94.50) | 130.50 (118.5) |
Data expressed as either mean ± standard deviation or median (interquartile range) as appropriate, except sex which has been expressed as frequency.
Out of the 162 enrolled patients, 29 died during admission, while four refused further treatment. A total of 129 patients were discharged from hospital. At three months, 32 patients had died and 91 patients were alive, out of which 54 patients were still dialysis-dependent. The remaining 37 patients had become dialysis independent. Only 12 out of these 37 patients had complete recovery. Seven patients underwent kidney biopsy during admission or follow-up. Acute pyelonephritis with severe acute tubular necrosis (n = 1), acute tubular necrosis (n = 2), diabetic glomerulosclerosis (n = 1), and crescentic glomerulonephritis with dominant chronic changes (n = 3) were biopsy diagnoses in these seven patients.
Overall, 61 (37.6%) patients died, 54 (33.3%) had persistent kidney failure requiring dialysis, 25 (15.4%) had incomplete recovery, and only 12 (7.4%) had complete recovery of kidney function.
This study highlights the outcomes after KDIGO stage 3 dialysis-dependent AKI in patients who were managed outside ICUs in resource-constrained settings. Over three months since admission, approximately one-third of patients had expired and another one-third had persistent kidney failure requiring dialysis. Complete recovery as judged by CKD-EPICr eGFR ≥60 ml/min/1.73m2 at three months after hospital discharge was seen in just 7.4%. These observations may be related to circumstances at study site. Being a tertiary care referral center, we often receive critically ill patients from other centers. Unfortunately, even after triage, some patients might continue to receive care (including dialysis) in the waiting areas for hours to days before subsequent transfer to medical wards or ICUs. This scenario highlights the real-life practical barriers to the implementation of visions like AKI 0 by 25 of the International Society of Nephrology (ISN). In view of the shortage of vacant beds and associated circumstantial compulsions, it was likely that patients who would have been deemed to have poorer prognosis (on account of very severe illness, multi-organ failure, advanced age, or comorbidities) would have been accorded lower priority for admission into ICUs or high dependency units. We have not objectively documented this or the overall quality of care, but these would be important considerations while interpreting results. However, we must note that 38% of participants did not report any comorbidity or preexisting illness. A recent publication describing the need and design of portable automated bag and mask ventilation device from our center appropriately highlights the huge gap between healthcare services burden and resources in our settings.5 Therefore, our study population might have had higher proportional representation of critically ill patients when compared to others.
A countrywide survey of AKI in China showed that only 59.3% of the 896 patients with indications for dialysis received it.6 Older age, male gender, severe comorbidities, being from lower-income area, or receiving treatment in local hospitals were associated with lower chances of being dialyzed despite indications for dialysis. Wang et al. also documented 25.1% mortality during hospital admission, 23.3% withdrawal from treatment, and 53.5% partial or complete renal recovery at discharge.6 Though this study’s settings, participant characteristics, event definitions, and follow-up were different from ours, the results do highlight the influence of nonclinical factors on outcomes. Our study explored outcomes in a unique setting, that is, receiving dialysis care outside critical care areas, a scenario that is otherwise widely prevalent in developing countries but has scant data. In 2017, the Acute Disease Quality Initiative (ADQI) meeting report that addressed AKI in developing regions emphasized the need for outcome data from low resource settings.S1 A study from Brazil did not find any difference between kidney replacement therapy for KDIGO stage 3 dialysis requiring AKI in ICU versus outside ICU settings.S2 Our study outcomes align closely with existing literature on dialysis-requiring KDIGO stage 3 AKI in high-risk populations with comorbidities.S3
There are certain limitations of our study. We have not recorded extensive clinical phenotype of the study population and temporal course of development of other complications. Patients who may have had dialysis indications but did not receive dialysis for any reason were not included. We do not have a corresponding group who received care in various ICUs for comparison. Our study population may not be reflective of the overall AKI that is seen at tertiary care centers. The population is likely to be skewed toward those who were presumed to be very sick with comorbidities at the time of admission. The relative high prevalence of patients with comorbidities reflects the same. Also, it may not have been fully possible to exclude milder forms of CKD in patients without any baseline data. Nevertheless, the description of broad kidney outcomes at three months in patients who were managed under such circumstantial compulsions may be pragmatic. Improving clinical outcomes in such circumstances is very challenging. The potential for novel or innovative implementation strategies in local context still exists and needs to be explored.
Financial support and sponsorship
International Society of Nephrology fellowship awarded to Dr. Onu Ugochi Chika.
Conflict of interest
There are no conflicts of interest.
References
- Acute kidney injury advisory group of the American society of nephrology. World incidence of AKI: A meta-analysis. Clin J Am Soc Nephrol. 2013;8:1482-93.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A systematic review and meta-analysis of acute kidney injury in the intensive care units of developed and developing countries. PLoS One. 2020;15:e0226325.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Global epidemiology and outcomes of acute kidney injury. Nat Rev Nephrol. 2018;14:607-25.
- [CrossRef] [PubMed] [Google Scholar]
- Community-acquired AKI in Asia: An update. Semin Nephrol. 2020;40:456-67.
- [CrossRef] [PubMed] [Google Scholar]
- Automatic AMBU bag operating device: Creating a boon for high-volume centres in low-income countries. BMJ Innovations. 2020;6:255-8.
- [Google Scholar]
- ISN AKF 0 by 25 China Consortium. Renal replacement therapy in acute kidney injury from a Chinese cross-sectional study: Patient, clinical, socioeconomic and health service predictors of treatment. BMC Nephrol. 2017;18:152.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







