Translate this page into:
Quality of Life of Children with Idiopathic Nephrotic Syndrome
Corresponding author: Jyoti Shukla, Nursing officer, Kalawati Saran Children Hospital, New Delhi, India. E-mail: jyoti_shukla1984@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Shukla J, Gupta A, Kalra R. Quality of Life of Children with Idiopathic Nephrotic Syndrome. Indian J Nephrol. 2025;35:234-42. doi: 10.25259/IJN_5_2024
Abstract
Background
Nephrotic syndrome (NS) is relapsing–remitting illness affecting children and characterized by proteinuria, edema, and hypoalbuminemia. The disease involves the significant formative years of a child’s life and profoundly impacts their physical and psychosocial well-being. There is a scarcity of literature exploring the quality of life (QoL) of children with NS and the factors influencing them. The study aimed to discuss the QoL of children with NS and the factors influencing it.
Materials and Methods
A systematic search of electronic databases, including PubMed, Google Scholar, and Embase, was carried out from 2004 to August 2023. Nineteen original articles in English language that focused on evaluating the QoL of children with NS were included. Articles in languages other than English, letters, and editorial reviews, studies involving populations other than children, were excluded.
Results
Children with NS tend to have a better QoL as compared to those with other chronic diseases (p = <0.001), but it remains lower than that of healthy children (p<0.05). School functioning was the most affected domain. Recurrent relapses, prolonged illness, high steroid dosages, and multiple medications are significant contributors to impaired QoL. Children with steroid-resistant nephrotic syndrome (SRNS) had poorer QoL among the clinical subtypes.
Conclusion
Children with NS face various challenges that impact their QoL. Comprehensive care strategies to enhance QoL are the need of the hour.
Keywords
Children
Nephrotic syndrome
Quality of life
Introduction
Nephrotic syndrome (NS) is the most common kidney disease among children marked by proteinuria, hypoalbuminemia, and edema. The prevalence is 16 cases per 100,000 and the incidence is 2–7 cases per 100,000 children.1 It is typically seen in children in the age group of 2–6 years, with a female-to-male ratio of 1:2.2,3 Higher incidence is seen among South Asian children.4
Prednisolone, an oral corticosteroid, is the drug of choice to treat primary nephrotic syndrome (PNS). About 60% to 70% of cases develop frequent relapses leading to decreased Quality of Life (QoL) and increased morbidity.5 The disease involves formative years of a child’s life impacting not only physical health but also psychosocial well-being.6 The QoL of children with NS may vary with disease clinical subtypes from infrequent relapsing to SRNS. NS exhibits a relapsing–remitting pattern, increasing the complexities of managing the multicomponent treatment regimens of the disease, including medication administration, dietary and lifestyle modifications, laboratory work, and follow-up, which may also have a substantial impact on the QoL.7 Understanding the QoL of children with NS is crucial for providing holistic care and improving patient outcomes.8
Very few studies explore the quality of life of children with NS, especially from developing countries. The current review explores the effect of disease conditions on the various domains of QoL and factors affecting QoL.
Materials and Methods
A comprehensive review of the literature was done. This review incorporates a systematic search of electronic databases, including PubMed, Google Scholar, and Embase from 2004 to August 2023. The Search terms included “Quality of life”, “Children”, “Nephrotic Syndrome”, “QoL”, and “Children with Nephrotic Syndrome”. Original articles exploring the QoL of children with NS were included. Non-English language articles, letters, and editorial reviews were excluded. Abstracts were evaluated, articles that focused on evaluating the QoL of children with NS were included, and populations other than children were excluded resulting in 19 studies, as shown in Figure 1.
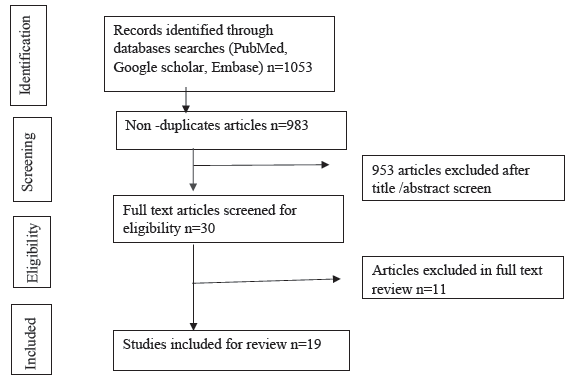
- Search strategy flow chart.
Many standardized tools have been used to evaluate the QoL of children with NS, such as the Pediatric Quality of Life Inventory 4.0 Generic Scale version (PedsQL), KINDLR Questionnaire, Child Health Questionnaire (CHQ), Generic Children`s Quality of Life Measure (GCQ) and Patient-Reported Outcomes Measurement Information System (PROMIS). The PedsQL 4.0 generic core scale has been the primary choice in majority of the studies.6,9-21 It includes physical, emotional, social, and school domains for different age groups (2–4 years, 5–7 years, 8–12 years, and 13–18 years). It comprises both child self-report and parent proxy-report, excluding the 2–4 year age group, which solely relies on parents’ reporting. Health-Related Quality of Life (HRQoL) is derived from the combined scores of all the domains, while psychosocial functioning is represented by cumulative scores of emotional, social, and school functioning. KINDLR questionnaire assesses various aspects of children and adolescent’s well-being and has physical parameters, emotional parameters, self-esteem, family, friends, school, and disease as its subscales. The tool has been employed in two distinct studies.22,23 GCQ is another instrument used in a single study along with PedsQL and measures the degree of satisfaction by comparing the perceived quality of life and the desired quality of life in oneself. High correlation is moted between GCQ and PedsQL scores.11 PROMIS encompasses domains such as depression, anxiety, social peer relationships, pain interference, fatigue, and mobility. A study employed PedsQL along with PROMIS and compared their consistency. A strong correlation was noted between PROMIS mobility, pain interference, fatigue, and the PedsQL physical functioning domain. A strong correlation was also observed between PROMIS depression and anxiety domain and the PedsQL emotional functioning scale. A moderate correlation (0.5 ≥ correlation coefficient > 0.3) was seen between the PROMIS peer relationship and PedsQL social and school functioning.6
Table 1 depicts the summary of studies included in the review. Veltkamp et al. investigated the QoL in children with first onset SSNS aged 2–16 years by PedsQL and revealed impaired QoL in children aged 8–18 years with SSNS.9 Kresnandari et al. observed that children not in remission and on cyclophosphamide therapy had a higher proportion of disturbances in QoL.14 Tanzina Parveen et al. reported better physical, emotional, and social functioning as compared to controls of children with other chronic illnesses.15 Allam et al. evaluated QoL of Sudanese children with NS and found significantly lower scores than healthy children as control except for social domain.16 Abbasi et al. assessed the QoL of Iranian children with NS and found reduced QoL compared to healthy children but better QoL as compared to children with other chronic illnesses.17 Aman et al. assessed the impact of the first pandemic wave on the QoL of children with NS and observed declined QoL in them.24 Mazahir et al. assessed QoL in children aged 2–18 years and found QoL scores were lower in healthy children.18 Aier et al. reported lower QoL in children with NS aged 6–12 years.19 Li et al. also reported similar findings of lower QoL in children with NS.20 Khullar et al. observed a decline in QoL of children using steroid and steroid-sparing agents.25 Menon et al. found better QoL in cases (children with NS who were in remission and off high-dose steroids) as compared to controls.22 Eid et al. evaluated Egyptian children with NS and observed better QoL as compared to children with other chronic illnesses but lower than healthy counterparts.11 Conversely, Roussel et al. reported that children in remission and on oral immunosuppressive drugs or rituximab therapy had high QoL.23 Solarin et al. also reported overall good QoL in children with NS in their setting.12 Rita Mbanefo et al. found worse QoL in the presence of edema, massive proteinuria, and steroid resistance in children with NS.13 Agrawal et al. found that QoL was better in children in NS as compared to children with other chronic illnesses.21 Rahman et al. reported QoL was worst affected in physical and social domains.10 Seleswki et al. assessed the impact of disease duration on QoL and found poor social and school functioning, peer relationships, and pain interference.6 Rüth et al. reported that social functioning was impaired.26
| Author and Year | Country | Purpose | Study design | Population | Sample size | Duration | Data collection tool | Findings |
|---|---|---|---|---|---|---|---|---|
| Veltkamp et al. (2023)9 | Netherland | To determine HRQoL in Children with first-onset SSNS | Cross-sectional prospective study | Children with SSNS aged 2–16 years, 4 weeks after onset of SSNS | 46 | 3 years 6 months | PedsQLTM4.0 (Dutch version) | A large proportion (>45%) of children (8-18 years) had impaired QoL, no differences in QoL (2-7 years) except for social functioning in (5-7 years) in comparison to the reference group. |
| Kresnandari et al. (2023)14 | Indonesia | To assess QoL in children with NS | Cross-sectional study | Children with NS aged 2–18 years | 60 | 6 months | PedsQLTM4.0 | Children with SRNS, SDNS and not in remission phase, on cyclophosphamide therapy demonstrate a higher proportion of QoL disturbance. |
| Tanzina Praveen et al. (2023)15 | Bangladesh | To assess QoL in children with minimal change nephrotic syndrome | Cross-sectional study, comparative |
Children with NS aged 2–18 years as cases Control-matched children attending general OPD or subspecialty clinic |
Cases – 50 Control – 50 |
6 months | PedsQLTM4.0 (Bangla version) | Children had significantly better scores in physical (p = 0.004), emotional (0.03), and social functioning (p = 0.01) as compared to controls. |
|
Allam et al. (2022)16 |
Sudan | To assess HRQoL in Sudanese children with NS | Case-control descriptive study |
Children with NS aged 2–18 years as cases Control-matched healthy children |
Cases – 100 Control – 100 |
8 months | PedsQLTM4.0 | Children with NS had lower QoL than healthy children (p ≤ 0.05) except social domain (p = 0.266). Children with the first episode of NS had lower QoL (p = 0.027) among the clinical phenotypes of NS. |
| Abbasi et al. (2022)17 | Iran | To assess health QoL in Iranian children with NS | Cross-sectional study, case-control study | Children with NS aged 6–18 years |
Cases – 60 Control I – 81 Control II – 98 |
- |
PedsQLTM4.0 (Farsi version) |
Children with NS had lower scores in physical, social, and educational fields as compared to healthy controls, but higher than children with other chronic diseases (p < 0.05) |
| Aman et al. (2022)24 | Canada | To assess the family functioning and parental and child QoL during the pandemic compared to pre-pandemic assessment | Prospective cohort | Children with aged 2–18 years | 122 | 5 months | PedsQLTM4.0 | Children’s overall QoL declined (p = 0.04), specifically increased sleep disruption (p = 0.01) and fatigue |
|
Mazahir et al. (2022)18 |
India | To assess QoL in children with NS | Cross-sectional study |
Children with NS aged 2–18 years Children visiting the hospital for minor acute illness |
102 cases and 102 control | 3 months |
PedsQLTM4.0 (Hindi version) |
Compared to controls, QoL scores were lower in physical (p<0.0001), school (p<0.026), and social domains (p <0.0001). SRNS had worse QoL. Older age at enrolment (p=0.016) and a higher number of immunosuppressants (p=0.015) are associated with impaired QoL. Cases with edema and CNI use are linked with impaired emotional (p-0.028) and social functioning (p-0.040). No difference in emotional functioning. |
| Aier et al (2022)19 | India | To assess emotional and behavioral problems, temperament, family environment, and health-related QoL in children with NS | Cross-sectional study | Children with NS aged 6–12 years |
32 cases 30 controls |
1 year | PedsQLTM4.0 | Children with NS overall lower QoL (p<0.003). SRNS had poor QoL scores (p<0.017). |
|
Li et al. (2021)20 |
China | To assess the QoL of children with NS and assess parental disease awareness | Survey | Children with NS hospitalized in a nephrology ward | 231 children | 20 months |
PedsQLTM4.0 (Chinese version) |
93.51% of cases had affected QoL. Longer duration of illness associated with impaired physical functioning pain and fatigue. |
| Khullar et al. (2021)25 | Canada | To assess the impact of steroids and steroid-sparing agents on the QoL of children with NS | Longitudinal cohort study | Children with NS aged 1–18 years |
295 Children with the incident and prevalent children with NS |
5 years |
PedsQLTM4.0 (Chinese version) |
Reduction in overall QoL for both steroid and steroid-sparing agents. Longer periods of medications over 6 months significantly lower QoL. Steroid-sparing agents associated with a reduction in general, sleep, and cognitive fatigue domains. |
|
Menon et al. (2020)22 |
India |
To assess the QoL of children with NS and their caregivers. To study behavioral abnormalities |
Cross-sectional study | Children with NS aged 4–15 years and controls were children with minor illnesses |
38 children with NS 41 healthy children as control |
18 months |
KINDLR SDQ, WHO-QoL BREF |
QoL was better in cases as compared to controls (p<0.003). Low emotional and peer domain was associated with complications of disease and adverse disease events. |
| Eid et al. (2020)11 | Egypt | To evaluate QoL in Egyptian children with NS | Cross-sectional study |
Children with NS as cases (8–18 years) Healthy children as control group I and children with other chronic illnesses as control group II |
300 100 cases and 100 controls in each group |
12 months |
PedsQLTM4.0 (Arabic version) Generic Children’s QoL measure (GCQ) |
QoL was better in children with NS as compared to children (p<0.001) with other chronic illnesses but lower than the healthy control (p<0.001) reported by PedsQL and similarly for GCQ (p = 0.02, p = 0.006), respectively. SRNS children had worse QoL (p≤0.001). Longer duration of illness, higher relapses, increased hospital admissions, and high cumulative glucocorticoid doses were associated with poor QoL (p<0.001 for all). |
| Roussel et al. (2019)23 | France | To assess the QoL of children with NS based on treatment modalities | Cross-sectional study/multicenter, observational study | Children with NS aged 7–17 years | 110 children | - | KindlR questionnaire |
Global QoL was high in children with difficult-to-treat NS in stable remission on oral immunosuppressive or Rituximab treatment. School function was impaired in the rituximab group. |
|
Solarin et al. (2019)12 |
Nigeria | To assess the QoL of children with INS | Cross-sectional study |
2–18 years Children with INS |
61 | 6 months | PedsQLTM4.0 | Overall QoL of children with NS was good. |
| Rita Mbanefo et al. (2018)13 | Nigeria | To assess the HRQoL of children with NS and the possible predictors of poor scores | Cross-sectional study | 5–18 years children with INS | 50 | - | PedsQLTM4.0 | Edema (p = 0.0006), massive proteinuria(p = 0.001), steroid resistance (p = 0.001), and non-MCNS (p = 0.012) negatively affect the QoL. |
| Agrawal et al. (2017)21 | India | To assess QoL in children with NS | Cross-sectional comparative study and children with other chronic illnesses as controls | Children with NS aged 2–18 years |
100 children 50 cases and 50 controls |
3 months | PedsQLTM4.0 (Tamil) |
QoL was better than controls (p = 0.012) and higher in physical (p = 0.004), emotional (p = 0.029), and social functioning (p = 0.010) as compared to controls. No difference in the school domain was noted. |
| Rahman et al. (2016)10 | Bangladesh | To assess QoL in children with NS | Cross-sectional study | Children with NS aged 2–12 years | 50 children with NS | 6 months |
PedsQLTM4.0 (Bengali) |
Physical (p<0.001) and social functioning (p = 0.003) were worst affected. |
|
Seleswki et al. (2015)6 |
USA | To assess the impact of disease duration on QoL in children with NS | Cross-sectional study | Children with NS aged 8–17 years | 127 children | - |
PROMIS PedsQLTM4.0 |
Disease duration impacts the QoL. Poor social (p<0.01) and school functioning(p = 0.03) reported by PedsQL and impaired peer relationship (p = 0.01) and pain interference (p<0.01) by PROMIS. |
|
Rüth et al. (2004)26 |
Netherland Switzerland Germany |
To assess QoL and psychosocial adjustment in SSNS | Cross-sectional study | Children with NS aged 3–19 years | 45 children | - | TNO-AZL child QoL questionnaire | Social functioning was impaired. |
HRQoL: Health-related quality of life, PedsQL: Pediatric quality of life inventory, PROMIS: Patient reported outcomes measurement information system, QoL: Quality of life, SDNS: Steroid dependent nephrotic syndrome, SSNS: Steroid-Sensitive nephrotic syndrome, SRNS: Steroid resistance nephrotic syndrome, SDQ: Strengths and difficulties questionnaire, TNO-AZL: The netherlands prganization for applied scientific research academical medical center, NS: Nephrotic syndrome
Impact on QoL of children with NS
The QoL was found to be better in children with NS in comparison to children with other chronic diseases. The median total QoL scores in children with NS were 65 (Interquartile range: 59–68.75) which was higher as compared to controls 62.19 (Interquartile range:58.05–65.78) (p = 0.012) with other chronic diseases such as epilepsy, asthma, hemophilia, etc.21 In other studies, it was consistently found that children with NS had higher mean total quality of life (QoL) scores compared to those with chronic non-renal illnesses, as measured by PedsQL (p = <0.001) and GCQ (p = 0.02).11,15 Both the studies were comparative and cross-sectional. Another study conducted on children who were in remission and not on high-dose steroid therapy affirmed better QoL compared to healthy controls by KindlR questionnaire (p = 0.003).26 While the QoL was noted to be better in comparison to children with nonrenal chronic illnesses, it remained lower than that of healthy children. Studies reported that mean total PedsQL scores were lower in NS children compared to healthy controls (p = 0.0004, p ≤0.05, and p ≤ 0.001, p ≤ 0.003, respectively).11,17-19 Children with NS reported that they experienced a decline in QoL (p = 0.04) during the initial pandemic wave, particularly increased sleep disruption and reduced energy (p = 0.01).24
Physical health
Physical functioning was reported to be poor in children with NS as measured by PedsQL.6,12,16-18 Children did not encounter issues with light activities, such as walking over 100 meters. They faced challenges when engaging in moderate or strenuous activities like running, sports, bathing, and household chores. Over half of them reported feeling pain and fatigue during these activities.20 Pain interference was also found to be more pronounced (p < 0.01) in children. Children with prevalent NS exhibited a higher degree of pain interference (p = 0.02) compared to those with incident NS.6 Physical functioning was reported to be better than children with other chronic diseases.21 Children with NS exhibited lower physical scores (68.26 ± 19.94) than healthy children (81.25 ± 18.40), p = <0.010.19 Another study reported a parallel outcome (p < 0.0001).18 The presence of edema significantly lowered physical scores (66.35 ± 19.65,p = .001).13
Psychosocial well-being
Psychosocial functioning encompasses the emotional, social, and psychological experiences of the children, and the disease course can significantly influence it. The psychosocial functioning of children with NS was also found to be impaired (65.52 ± 14.72) as compared to healthy children (74.88 ± 12.35) p < 0.10.19
Emotional Functioning: Children with NS exhibit higher emotional functioning as compared to children with other chronic diseases (p = 0.029, p = 0.03).15,21 No difference was noted in emotional functioning as compared to healthy controls.18 The emotional functioning of patients with NS also remained unchanged from their nonhealthy controls (p > 0.5).17 Children generally reported lower scores on sleep disturbances and expressed concerns about accidents.20 Minimal Change Nephrotic Syndrome (MCNS) also has better emotional functioning than non-MCNS (t = −4.272,p = 0.001).13 Instances with edema and ongoing or prior use of calcineurin inhibitor (CNI) were more prone to impaired emotional (p = 0.028) and social (p = 0.040) functioning.18 Children with SRNS exhibited diminished emotional functioning (65.75 ± 23.58) in comparison to those with SSNS (88.75 ± 22.61), with a statistically significant difference (p = 0.002).18
Social Functioning: Social functioning was observed to be better in children with NS as compared to other chronic illnesses.15 It was noted to be impaired in children with NS as compared to healthy controls (p = 0.026).18 Conversely, a study reported that social functioning was better in cases as compared to healthy control (p<0.05).16 It was more compromised in prevalent patients (p<0.01) by PedsQL and in the peer relationship domain (p = 0.01) by PROMIS.6 While overall, social functioning was found to be better, some challenges were reported in getting along with other teenagers, making friends, and being teased by others.20
School domain
Studies have shown that school functioning is the most adversely affected domain among children with NS.6,12,16-18,20 Children experienced more significant impairment (p < 0.0001) in comparison to their healthy controls.18 Despite experiencing chronic absenteeism or dropping out from schooling due to the disease, children with NS also encounter challenges related to attention and memory.20 The presence of edema, particularly in the legs and ankles, limits a child’s mobility and significantly affects school functioning (46.54 ± 14.77, p = 0.002).13 Prevalent patients exhibited worse school functioning domains (p = 0.03).6 Based on the treatment modalities, school functioning was poor (p = 0.033) in the rituximab (RTX) group as compared to the oral immunosuppressive drugs (OID) group. It may be due to repeated hospitalization for infusion or monthly B-Cell monitoring.23 Only a single study reported that no difference was noted in the school domain as compared to children with other chronic diseases.15
Factors affecting QoL
NS significantly impacts children’s QoL, influenced by various factors such as psychosocial, cultural, socioeconomic, and educational aspects.Children with prevalent disease have poorer QoL than those with incident disease.6 Increased number of immunosuppressants used (p = 0.015) are the main predictors of impaired QoL.18 The use of steroids and steroid-sparing agents up to 12 months before assessment was linked to declined QoL which remained significant even after adjusting for factors.25
A longer duration of illness, a greater number of medications, frequent relapses, and high cumulative steroid doses are all linked to a lower QoL (p < 0.001 for all) for both PedsQL and GCQ.11 The relapsing type of NS, gender, duration of illness, average annual hospital admissions, body weight and obesity, cushingoid complications, and CNI use significantly affect the QoL scores in patients with NS (p<0.05).17 Age, gender, duration of illness, steroid resistance, complications, per capita income, and history of peritonitis did not significantly influence the QoL scores among children with NS (p>0.05).11,15,21
Duration of less than 1 year of illness adversely impacted physical functioning (p = 0.002) of children compared to those exceeding 1 year of illness. Conversely, emotional functioning showed improvement in children with an illness duration of less than 1 year (p = 0.035).13
QoL scores considerably differed between various clinical phenotypes of NS as patients experiencing initial episodes of NS had the lowest scores compared to other clinical phenotypes (p<0.05).16 SRNS group had the lowest scores in all domains compared to other clinical phenotypes (p ≤ 0.001, p = 0.017).11,19 Studies reported that no significant difference was found in the QoL of various clinical phenotypes of NS (p>0.05).15,17,21 The first episode or infrequent relapsing NS has a more favorable outcome in emotional, social, and school functioning as compared to FRNS/SDNS and SRNS.18
A proteinuria level of 3+ was also observed to be associated with a reduction in QoL across physical (F = 8.228, p < 0.001), social (F = 4.377, p = 0.009), and school (F = 12.815, p < 0.001) domains when compared to individuals with lesser degrees of proteinuria.13 Edema, massive proteinuria, steroid resistance, and non-MCNS histology types contribute adversely to QoL. Children with MCNS histology type experienced a significantly better QoL (87.19 ± 6.72) as compared to those with non-MCNS (74.82 ± 12.82), p = 0.012.13
Challenges experienced by children with NS
There are limited studies that have explored the QoL in children with NS, particularly in the context of developing countries. Several standardized instruments have been employed to assess the QoL of children with NS, including the PedsQL, GCQ, KindlR questionnaire, and PROMIS. Notably, the PedsQL stands out as the predominant choice in the majority of research studies.6,8-20
Children with NS often experience a range of physical symptoms, including edema and fatigue, and are susceptible to infections which can impact their physical QoL. It may make walking, running, and playing more challenging. Children may also experience fatigue due to the loss of vital proteins in the urine. Edema, particularly in the legs and ankles, can cause discomfort, which limits a child’s mobility and is found to be significantly affecting physical functioning.13
The fear of relapses and uncertainty about the future are significant emotional stressors.18 It can lead to anxiety, depression, and a decline in self-esteem among children with NS. In addition, medications used to manage NS, such as corticosteroids, can have side effects like weight gain, mood swings, and increased appetite, and these side effects may affect a child’s physical appearance and emotional well-being. Steroid-sparing agents are also associated with a reduction in general, sleep, and cognitive fatigue domains.25
Social and school domains are interrelated as school attendance provides an opportunity to interact with peers and make friends. Social isolation and school-related challenges can also affect the social functioning of these children. Poor school performance could be attributed to frequent hospital visits due to disease conditions and adverse effects of medications. With the remitting–relapsing nature of the disease, children find it difficult to attend school regularly and cope with their studies. In addition, a punitive school environment and teachers’ inadequate knowledge about the disease posed a barrier to preventing integration into the school domain leading to chronic absenteeism or dropping out of school. It is high time to acknowledge the vital role of peer support and raise awareness about the disease. It isimportant to recognize that factors such as ethnicity, culture, social practices, and socioeconomic status predominantly influence the social and emotional aspects of the QoL in children with chronic diseases. Therefore, making broad generalizations based on these findings would be inadequate.
The disease requires ongoing management, including medications, dietary restrictions, and laboratory assessments as each relapse (presence of 3+ or more proteins in the urine for 3 days in a row) carries a risk of morbidity, and steroid toxicity increases the possibility of complications like sepsis, thrombosis, malnutrition, etc.6 Dietary modifications may improve the health outcomes in children.27 However, adherence to the treatment plan and adapting to lifestyle changes can be challenging and often contribute to a reduced QoL.26 A study found that children with less than 1 year of illness had poorer physical functioning compared to those with more than 1 year of illness. This difference could be because of the challenges in adjusting to new symptoms over a shorter period. In contrast, emotional functioning was worse in children with an illness duration exceeding 1 year. This might be attributed to frequent relapses and changes in physical appearance, such as cushingoid facies and obesity, among other factors.13 The steroids and steroid-sparing agents lead to a decline in overall QoL due to the potential side effects of steroids and other immunosuppressive agents. A significant number of children with SSNS exhibited binge eating as a side effect of prednisolone followed by moon facies.9 Understanding and addressing these factors is essential for improving the overall well-being of these children.
Gaps and future research directions
There are limited studies that have explored the QoL in children with NS, particularly in the context of developing countries. Several standardized instruments have been employed to assess the QoL of children with NS, including the PedsQL, GCQ, KindlR questionnaire and PROMIS. Notably, the PedsQL stands out as the predominant choice in the majority of research studies.6,8–20
While the existing literature explored the QoL of children with idiopathic nephrotic syndrome were mostly comparative and cross-sectional. There is a need for a longitudinal study to track QoL changes over time, and interventional studies to enhance QoL. Most of the studies used the PedsQLTM4.0 generic core scale as the tool to assess QoL. It is essential to incorporate alternative assessment tools to enrich our understanding of QoL.
The QoL of children with NS is a multifaceted construct encompassing physical, emotional, and social dimensions. Comprehensive care strategies that address not only the physical symptoms but also the psychosocial well-being of these children and their caregivers are essential. Future research should aim to fill existing gaps, provide a longitudinal perspective, and develop targeted interventions to improve the QoL of this vulnerable population. Ultimately, enhancing the QoL of children with NS can lead to better health outcomes and improved overall well-being.
Conflicts of interest
There are no conflicts of interest.
References
- Steroid sensitive nephrotic syndrome. In: Pediatric kidney disease 2017. Berlin, Heidelberg: Springer Berlin Heidelberg; 2017. p. :419-53.
- [Google Scholar]
- Time trends and ethnic patterns of childhood nephrotic syndrome in Yorkshire, UK. Pediatr Nephrol. 2001;16:1040-4.
- [CrossRef] [PubMed] [Google Scholar]
- Steroid-sensitive nephrotic syndrome in children: Triggers of relapse and evolving hypotheses on pathogenesis. Ital J Pediatr. 2015;41:19.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The impact of disease duration on quality of life in children with nephrotic syndrome: A Midwest pediatric nephrology consortium study. Pediatr Nephrol. 2015;30:1467-76.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pediatric self-management: A framework for research, practice, and policy. Pediatrics. 2012;129:473-85.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Exploring conceptual context for resilience assessment scale for children with renal diseases. Int J Nurs Educ. 2020;12:182-7.
- [Google Scholar]
- Health-related quality of life of children with first onset steroid-sensitive nephrotic syndrome. Eur J Pediatr. 2023;182:4605-14.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Health-related quality of life in children with nephrotic syndrome in Bangladesh. Mymensingh Med J. 2016;25:703-9.
- [PubMed] [Google Scholar]
- Health-related quality of life in egyptian children with nephrotic syndrome. Qual Life Res. 2020;29:2185-96.
- [CrossRef] [PubMed] [Google Scholar]
- Sat-316 health related quality of life of children with nephrotic syndrome in Lagos Nigeria. Kidney Int Reports. 2019;4:140.
- [Google Scholar]
- The clinical parameters affecting the health-related quality of life of children with nephrotic syndrome. Arch Nephrol. 2018;1:11-8. Available from: https://doi.org/10.22259/2639-3573.0101002
- [CrossRef] [PubMed] [Google Scholar]
- The quality of life in children with nephrotic syndrome at prof I.G.N.G Ngoerah hospital, denpasar, bali. Intisari Sains Medis. 2023;14:401-6.
- [Google Scholar]
- Quality of life in children with minimal change nephrotic syndrome. Glob Acad J Med Sci. 2023;5:138-43.
- [Google Scholar]
- Assessment of health-related quality of life in sudanese children with nephrotic syndrome: A questionnaire-based study. Pan Afr Med J. 2022;43:154.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Heath-related quality of life in iranian children with nephrotic syndrome. Iran J Pediatr. 2022;32:118426.
- [Google Scholar]
- Quality of life in children with nephrotic syndrome: A cross-sectional study using Hindi version of PedsQL 4.0 generic core scales. Clin Exp Nephrol. 2022;26:552-60..
- [CrossRef] [PubMed] [Google Scholar]
- Psychosocial functioning and health-related quality of life in children with nephrotic syndrome: Preliminary findings. . 2022;18:306-14.
- [Google Scholar]
- Evaluating the quality of life of 231 children with primary nephrotic syndrome and assessing parental awareness of the disease. Front Pediatr. 2021;9:745444.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Assessment of quality of life in children with nephrotic syndrome at a teaching hospital in South India. Saudi J Kidney Dis Transpl. 2017;28:593-8.
- [CrossRef] [PubMed] [Google Scholar]
- Behavioral problems, quality of life and caregiver burden in children with idiopathic nephrotic syndrome: Improving outcomes by pragmatic interventions in a resource-poor setting. Indian J Pediatr. 2021;88:476-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Quality of life in children with severe forms of idiopathic nephrotic syndrome in stable remission—A cross-sectional study. Acta Paediatr Int J Paediatr. 2019;108:2267-73.
- [CrossRef] [PubMed] [Google Scholar]
- Family functioning and quality of life among children with nephrotic syndrome during the first pandemic wave. Pediatr Nephrol. 2023;38:3193-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Impact of steroids and steroid-sparing agents on quality of life in children with nephrotic syndrome. Pediatr Nephrol.. 2021;36:93-102.
- [CrossRef] [PubMed] [Google Scholar]
- Health-related quality of life and psychosocial adjustment in steroid-sensitive nephrotic syndrome. J Pediatr. 2004;145:778-83.
- [CrossRef] [PubMed] [Google Scholar]
- A Pre-experimental study to assess the effectiveness of structured teaching programme on knowledge regarding dietary modification among chronic kidney disease patients undergoing haemodialysis IJSRR. . 2019;8:2281-9.
- [Google Scholar]








