Translate this page into:
Rapidly progressive renal failure in a patient with extranodal non-Hodgkin's lymphoma
Address for correspondence: Dr. Raja Ramachandran, Department of Nephrology, Post Graduate Institute of Medical Education and Research, Chandigarh, India. E-mail: drraja_1980@yahoo.co.in
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A 60-year male was admitted with advanced renal failure and bilaterally enlarged kidneys. Kidney biopsy revealed diffuse interstitial infiltration by CD20 + lymphomatous cells suggestive of diffuse large B-cell, non-Hodgkin's lymphoma. Bone marrow examination was negative for malignant cells. Positron emission tomography-computed tomography showed uniformly diffuse and avid flurodeoxy glucose uptake in both kidneys, multiple hypodense areas of both lobes of liver, and axial and appendicular skeleton. Patient was treated with rituximab, cyclophosphamide, hydroxydaunorubicin, vincristine and prednisolone, became afebrile and serum creatinine normalized.
Keywords
Primary renal lymphoma
complication
rapidly progressive renal failure
Introduction
In various autopsy series, renal involvement is reported in 30-50% of patients with lymphoma.[1] Primary renal lymphoma (PRL) constitutes 0.1-0.7% of all extranodal lymphomas.[2] Renal failure due to lymphomatous infiltration is rare. We present an unusual case of PRL with advanced renal failure.
Case Report
A 60-year-old male with type 2 diabetes mellitus of 5 years’ duration, on oral hypoglycemic drugs with good control of blood sugars and documented coronary artery disease with a baseline serum creatinine of 1.2 mg/dl, presented with intermittent fever, weight loss and anorexia of 2-month duration. There was no alteration in bowel habits, ecchymosis, purpura, chronic cough, long-standing headache and pain abdomen. On examination, he was hemodynamically stable, pallor was present and there was no edema or lymphadenopathy. Per-abdomen, cardiovascular and respiratory system examinations were unremarkable. On evaluation, he had hemoglobin of 8 g/dl and peripheral smear showed normocytic and normocytic picture. Total leukocyte and platelet counts were 6900/μl and 2.5 × 105/μl, respectively. Alanine transaminase, aspartate transaminase, serum albumin, total bilirubin and alkaline phosphatase were 28 U/L, 16 U/L, 4 g/dl, 0.4 mg/dl and 97 U/L, respectively. Renal functions were deranged with serum creatinine and blood urea nitrogen of 8.5 mg/dl and 235 mg/dl, respectively. However, his urine output was adequate. Serum uric acid was high (13 mg/dl) and lactate dehydrogenase was elevated (1400 IU/dl). Serum protein electrophoresis didn’t reveal monoclonal proteins. Urine analysis showed 1+ albumin and no red blood corpuscles or white blood cells. Twenty-four hour urinary protein was 500 mg/dl. Ultrasound of kidney ureter bladder showed right kidney of 12.3 cm and left kidney of 12.4 cm with echogenic contents suggestive of calculi. Both kidneys were globular in outline with raised cortical echotexture. Antinuclear antibody (by immunofluorescence), anti-neutrophilic cytoplasmic antibodies (by immunofluorescence and ELISA) were negative. Complement factor 3 and 4 were 108 mg/dl and 44 mg/dl, respectively. Hepatitis B surface antigen, human immunodeficiency virus-I/II and anti-hepatitis C viral serology were negative. With a provisional diagnosis of rapidly progressive renal failure (RPRF), kidney biopsy was done.
Histopathological examination revealed [Figure 1a] diffuse interstitial infiltration with lymphomatous cells with morphology suggestive of high-grade non-Hodgkin's lymphoma (NHL) and immunohistochemistry showed [Figure 1b] CD20 positivity of the lymphomatous cells, suggestive of diffuse large B-cell, non-Hodgkin's lymphoma (DLBCL). To further characterize the disease, positron emission tomography-computed tomography (PET-CT) was done, which demonstrated avid flurodeoxy glucose (FDG) uptake in enlarged left and right kidneys with standardized uptake value (SUV) max of 18.5 and 9.5, respectively. A note was made of 9 mm calculus in left kidney lower calyx. Avid FDG uptake was also seen in multiple hypodense areas in both lobes of liver (SUV max 13.8), largest being 7.9 cm × 5.5 cm in the left lobe [Figure 2] and intense patchy uptake in the bone marrow of multiple bones in axial and appendicular skeleton. Bone marrow examination did not reveal any infiltration with lymphomatous cells. Patient was diagnosed as extranodal NHL, in the form of PRL with RPRF and secondary hepatic involvement. His disease was staged as IV BE according to Ann Arbor staging system and his international prognostic index score was 5/5. Chemotherapy was initiated with rituximab, cyclophosphamide, hydroxydaunorubicin, vincristine and prednisolone (R-CHOP) regimen. Twenty days post-chemotherapy, patient's well-being improved; he became afebrile and his serum creatinine came down to 1.2 mg/dl from 8.5 mg/dl.
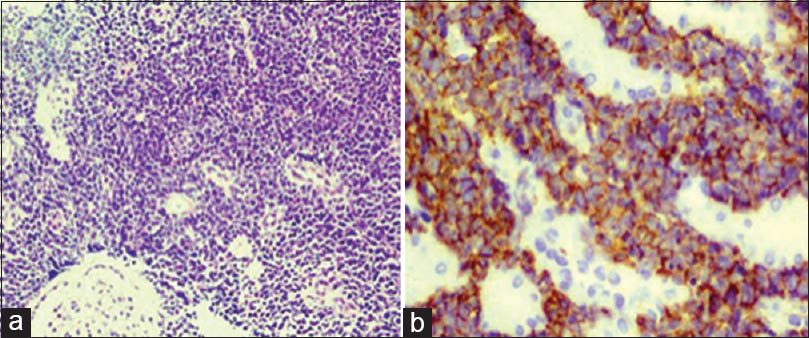
- Photomicrographs from the kidney biopsy specimen. (a) Diffuse interstitial infiltration by lymphomatous cells (H and E, ×200), (b) Immunohistochemistry showing diffuse membranous positivity for CD20 of the lymphomatous cells
![Positron emission tomography - computed tomography imaging. (a) Increased flurodeoxy glucose (FDG) uptake (standardized uptake value [SUV] max 9.5) is noted in the right kidney with regular margins. Increased FDG uptake is also noted in left kidney (SUV max 18.5) with irregular margins. Note is made of 9 mm calculus in left kidney lower calyx with mild hydronephrosis. (b) Avid FDG uptake is noted in multiple lesions in liver with largest lesion (7.9 cm × 5.9 cm, SUV max 13.8) in left lobe](/content/170/2015/25/1/img/IJN-25-43-g002.png)
- Positron emission tomography - computed tomography imaging. (a) Increased flurodeoxy glucose (FDG) uptake (standardized uptake value [SUV] max 9.5) is noted in the right kidney with regular margins. Increased FDG uptake is also noted in left kidney (SUV max 18.5) with irregular margins. Note is made of 9 mm calculus in left kidney lower calyx with mild hydronephrosis. (b) Avid FDG uptake is noted in multiple lesions in liver with largest lesion (7.9 cm × 5.9 cm, SUV max 13.8) in left lobe
Discussion
Renal involvement of the lymphoma can occur in various ways. In almost all cases, it appears to be a secondary process, either by direct extension from a retroperitoneal mass or via hematogenous spread in the setting of a disseminated disease.[3] By definition, the term PRL is applied to patients with disease localized to the kidney without any sign of other organ involvement or in whom renal involvement is the presenting manifestation.[4] It is rare and some investigators doubt presence of PRL. Kandel et al. had shown that out of 17 cases of PRL who underwent autopsy, all the patients had evidence of extra-renal disease.[5] Interpretation of these data had led to the conclusion that primary lymphoma of the kidney does not exist. However, Okuno et al. reviewed 176 cases of NHL with renal involvement and were able to identify 5 cases that met the criteria for PRL.[6] There is still debate on whether tumor invades the renal parenchyma from adjacent lymph nodes or whether the lymphomatous process originates within the kidney. Hematological malignancies presenting with acute kidney injury (AKI) include plasma cell dyscrasia (most common being multiple myeloma), chronic myeloid leukemia with blast crises, chronic myelomonocytic leukemia with leukemic infiltration and acute myelogenous leukemia.[7]
Our patient had PRL, as there was no lymph nodal involvement on imaging and despite radiological evidence of hepatic and bone marrow involvement patient did not have hepatic dysfunction or marrow involvement of lymphoma on bone marrow examination. There are several mechanisms of renal failure in patients with lymphoma, which include ureteral obstruction, hypertension from compression of renal vessels, urate nephropathy, hypercalcemia, sepsis, volume depletion, paraproteinemia and immunologically mediated glomerular injury.[8] In the present case, CT scan ruled out obstructive uropathy and reno-vascular disease. Hypercalcemia, volume depletion, sepsis and paraproteinemia induced AKI as patient's serum calcium level was normal (9.2 mg/dl). On clinical examination, there was no evidence of volume depletion (central venous pressure was 10 cm of normal saline) and sepsis (leukocyte count was 6900), and serum electrophoresis did not reveal any monoclonal protein and the light chain assay was normal adjusted to renal failure (κ:λ =2). Immunofluorescence on the kidney biopsy specimen did not reveal any evidence of immunologically mediated disease. However, renal failure due to infiltration of the kidneys by DLBCL is an unusual manifestation and also a rare presenting symptom of a hematological malignancy. Until now, only case reports were published in the literature regarding this manifestation.[89] Our patient presented with RPRF due to infiltration by lymphomatous cells, which was proved on histopathological examination. Renal lymphoma has a wide variety of imaging patterns. The most common imaging appearance of renal lymphoma is that of multiple parenchymal masses of variable size. Other patterns include solitary renal mass, bilateral renal enlargement, and peri-renal soft tissue masses.[10] Both contrast-enhanced CT and MR imaging are superior to ultrasonography in detecting the presence of disease as well as the number of renal lesions and the presence of extra-renal tumors.[11] Combined PET-CT allows precise localization and potential earlier detection of additional tumor foci. In our patient, PET-CT showed activity in kidneys, liver and bone marrow of axial and appendicular skeleton. Despite this, there was no malignant cells detected on bone marrow examination and there was no hepatic dysfunction.
Systemic chemotherapy with or without radiotherapy is a widely used treatment for PRL, as well as the option of surgery in the case of PRL affecting one kidney.[12] Bilateral renal lymphomas are usually treated by aggressive chemotherapy as frontline therapy. This approach could preserve the organ function, but generally the prognosis is poor. Because of the low incidence of this disease, randomized studies aiming to compare different therapy approaches have not been reported. Our patient's renal function normalized with R-CHOP chemotherapy regimen. Prognosis is poor in patients with PRL. They succumb to their illness either due to recurrence or due to infection. Cupisti et al. mentioned that out of 34 cases with bilateral renal involvement by lymphoma, only 11 patients achieved remission and the remaining died.[2] The present report is limited by short-term follow-up of the patient.
In conclusion, PRL is one of the rare causes of RPRF and the renal dysfunction would reverse on prompt management with appropriate chemotherapy.[13]
Source of Support: Nil
Conflict of Interest: None declared.
References
- Renal involvement in patients with non-Hodgkin's lymphoma: Clinical and pathological features in 23 cases. Hematol Oncol. 1990;8:105-10.
- [Google Scholar]
- Bilateral primary renal lymphoma treated by surgery and chemotherapy. Nephrol Dial Transplant. 2004;19:1629-33.
- [Google Scholar]
- Diffuse large B-cell lymphoma with involvement of the kidney: Outcome and risk of central nervous system relapse. Haematologica. 2011;96:1002-7.
- [Google Scholar]
- Lymphoma of the kidney: Primary or initial manifestation of rapidly progressive systemic disease? Int Urol Nephrol. 2006;38:775-8.
- [Google Scholar]
- Primary renal non-Hodgkin's lymphoma. An unusual extranodal site. Cancer. 1995;75:2258-61.
- [Google Scholar]
- Acute renal failure due to lymphomatous infiltration: An unusual presentation. Saudi J Kidney Dis Transpl. 2006;17:395-8.
- [Google Scholar]
- Acute renal failure and bilateral kidney infiltration as the first presentation of non-Hodgkin lymphoma. Iran J Kidney Dis. 2009;3:50-3.
- [Google Scholar]
- Imaging of renal lymphoma: Patterns of disease with pathologic correlation. Radiographics. 2006;26:1151-68.
- [Google Scholar]
- Bilateral solid multifocal intrarenal and perirenal lesions: Differentiation with ultrasonography, computed tomography and magnetic resonance imaging. Clin Radiol. 1995;50:288-94.
- [Google Scholar]
- Primary bilateral T-cell renal lymphoma presenting with sudden loss of renal function. Nephrol Dial Transplant. 2001;16:1487-9.
- [Google Scholar]
- Non-Hodgkin lymphoma mimicking renal carcinoma: Apropos of 1 case of follicular lymphoma. Ann Pathol. 2000;20:253-7.
- [Google Scholar]







