Translate this page into:
Renal Allograft Malakoplakia: Favorable Outcome with Early Diagnosis and Prolonged Antibiotic Therapy
Corresponding author: Kalathil K Sureshkumar, Division of Nephrology and Hypertension, Medicine Institute, Allegheny General Hospital, Allegheny Health Network, Pittsburgh, PA, United States. E mail: kalathil.sureshkumar@ahn.org
-
Received: ,
Accepted: ,
How to cite this article: Sureshkumar KK, Daloul R, Nashar K. Renal Allograft Malakoplakia: Favorable Outcome with Early Diagnosis and Prolonged Antibiotic Therapy. Indian J Nephrol. doi: 10.25259/IJN_98_2025
Dear Editor,
Malakoplakia is an granulomatous inflammatory disorder generally associated with Escherichia coli infection in immunocompromised hosts.1 It affects the urinary tract, especially the bladder. Renal parenchymal involvement is rare. The underlying defect could be impaired bactericidal ability of macrophages.2 Before 1990, malakoplakia had a poor prognosis and higher mortality, but antibiotics with higher intracellular penetration, e.g., quinolones improved the outcomes.3
A 36-year-old female on tacrolimus/mycophenolate mofetil (MMF) maintenance, who had live-donor kidney transplantation 4 years ago, was admitted with malaise, back pain, and nausea. Her baseline serum creatinine was ∼1.3 mg/dL. Two weeks earlier, the patient developed Escherichia coli allograft pyelonephritis, bacteremia, and acute kidney injury and was given a 3-week oral ciprofloxacin course. MMF was stopped.
Urine and blood cultures and serum CMV, BK, and EB virus PCRs were all negative. CT imaging showed persistent renal allograft swelling. Renal allograft biopsy showed normal glomeruli, with 70% of renal parenchyma showing histiocytic predominant inflammatory infiltrates (von Hansemann cells) and neutrophilic tubulitis on light microscopy [Figure 1a]. Von Kossa stain showed Michaelis-Gutmann bodies [Figure 1b]. SV-40 and peritubular capillary C4d stains were negative. Immunofluorescence was unremarkable. Renal allograft malakoplakia was diagnosed based on the biopsy. The patient responded favorably to immunosuppression reduction and prolonged antibiotics, including IV ceftriaxone (6 weeks) followed by PO ciprofloxacin (8 weeks), with improvement in serum creatinine to 1.46 mg/dL at the final follow-up.
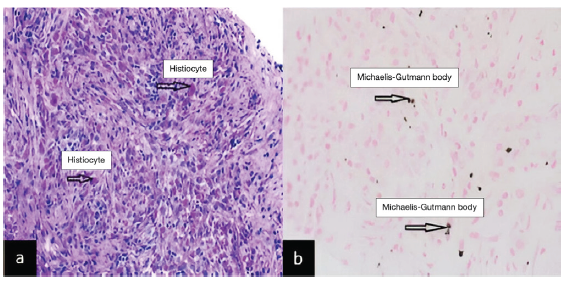
- (a) Light microscopy showing malakoplakia of the kidney allograft with distorted parenchyma and infiltrating PAS-positive histiocytes (black arrows), magnification x 100. (b) Von Kossa stain showing rounded Michaelis-Gutmann bodies (black arrows), magnification x 100.
Malakoplakia is a plaque-forming, non-neoplastic, locally destructive inflammatory disease. Michaelis-Gutmann bodies, pathognomonic in diagnosis, are derived from phagolysosomes containing incompletely destroyed bacteria.2 Renal allograft involvement is rare, with very high risk of allograft failure. High index of suspicion with an early histological diagnosis, reduction in immunosuppression, and prolonged antibiotic therapy could improve prognosis as in our patient.
Conflicts of interest
There are no conflicts of interest.
References
- Genitourinary malakoplakia in renal transplant recipients: Pathogenic, prognostic and therapeutic considerations. J Urol. 1984;132:10-12.
- [CrossRef] [PubMed] [Google Scholar]
- Renal malacoplakia reappraised. Am J Kidney Dis. 1993;22:243-52.
- [CrossRef] [PubMed] [Google Scholar]
- Ciprofloxacin for treatment of malakoplakia. Lancet. 1992;339:148-9.
- [CrossRef] [PubMed] [Google Scholar]






