Translate this page into:
Renal cortical necrosis in a renal transplant recipient
Address for correspondence: Dr. Venkatesh Ravi, #60, 2nd Main, 4th Cross, M.S.R. Nagar, Bangalore - 560 054, India. E-mail: venkateshravi.8711@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Renal cortical necrosis (RCN) is a rare cause of acute renal failure. We report the case of a 49-year-old male, who developed RCN 4 years after transplant.
The patient, who had type 2 diabetes and hypertension with chronic kidney disease, received a renal transplant from his wife. He was started on triple immunosuppression with cyclosporine, mycophenolate mofetil and steroids. Due to evidence suggestive of early cyclosporine toxicity on renal biopsy in initial post-transplant period, cyclosporine was replaced with everolimus. Patient was on regular follow-up with normal serum creatinine levels. Four years later, he presented with intermittent fever for 2 days and sudden onset breathlessness for 1 day which was associated with fatigue, nausea, vomiting, diffuse abdominal pain and lower limb swelling. He took acetaminophen for fever prior to presentation. On examination, he was drowsy but oriented to time, place, person with pulse rate of 86/min, blood pressure of 170/90 mmHg, respiratory rate of 26/min, and temperature of 99.4°F. He had bilateral pedal edema and moderate pallor, auscultation revealed bilateral crackles. He was stabilized in medical intensive care unit.
There was progressive deterioration in his renal function and he developed anuria. Serum creatinine level increased from 1.40 mg/dl on day 1 to 8.57 mg/dl on day 7. He was taken up for emergency hemodialysis through internal jugular venous (IJV) catheter. The measured drug levels of everolimus were within therapeutic limits and he was on adequate dose of mycophenolate mofetil and steroids. Renal biopsy [Figure 1] was suggestive of diffuse RCN. Sections showed multiple cores of renal tissue with extensive areas characterized by preservation of outlines of necrotic glomeruli and tubules with no zone of hyperemia. There was no evidence of thrombotic microangiopathy (TMA). C4d staining of the specimen was negative.[12] Test for donor specific antibodies was also negative.
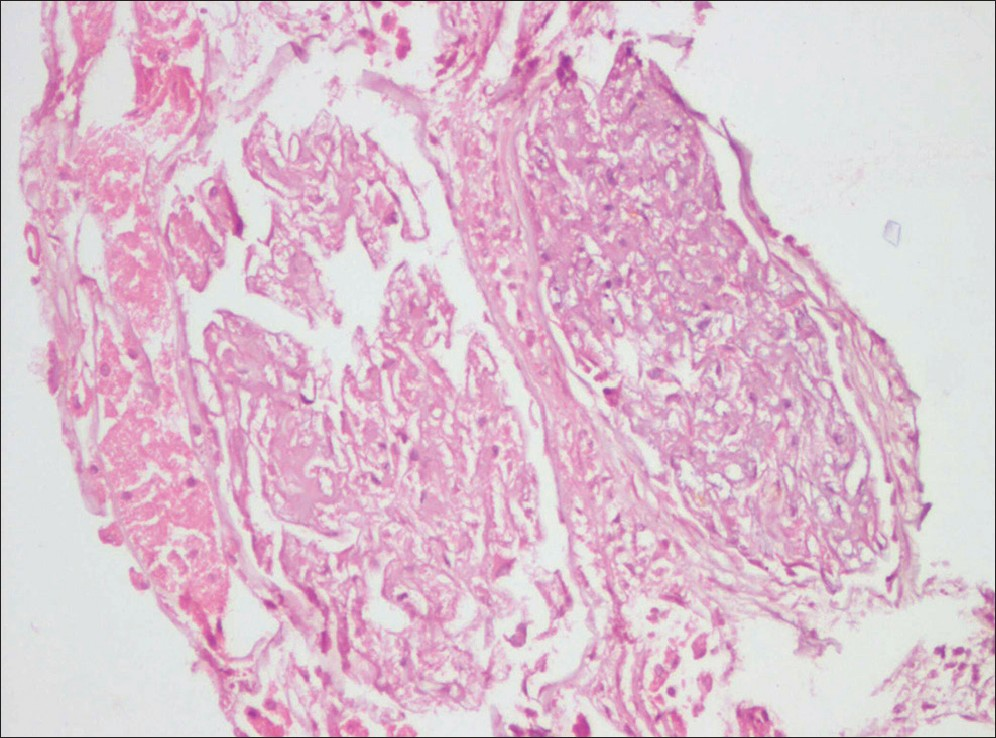
- Two completely necrotic glomeruli with adjacent necrotic tubules. (H and E, × 200)
This case did not exhibit any evidence of the traditional etiologies of RCN. Patient was on immunosuppression with everolimus following transplant. Everolimus is known to inhibit glomerular endothelial cell (GEN) proliferation and vascular endothelial growth factor.[34] This everolimus-induced anti-proliferative effect was also confirmed in GEN in vitro, showing that everolimus blocks proliferation of GEN incompletely to values found in non-stimulated cells. It has been demonstrated that everolimus has the potential to exacerbate the acute phase of glomerular endothelial injury in experimental rats, which is likely to occur in humans as well. Although this experimental model is characterized by a single-timed endothelial injury, endothelial injury during human disease is usually ongoing for a longer period of time.[3] The delay of the endothelial repair and transient glomerular hypocellularity during TMA is shown to be associated with increased glomerular fibrin indicating short-term disease aggravation.[3] Existing literature suggests that treatment with mammalian target of rapamycin inhibitors requires caution during active microangiopathy or acute humoral rejection, though it appears to be relatively safe once acute injury has subsided.[35] Hence, it is possible that everolimus could have aggravated some underlying acute injury in this post-transplant, acute febrile scenario leading to diffuse RCN in this patient.
The point of interest is the potential role of everolimus in exacerbation of acute renal injury which needs to be evaluated further to have more definitive evidence and guidelines regarding this effect.
References
- The impact of C4d staining as a humoral injury marker. Transplant Proc. 2012;44:1694-6.
- [Google Scholar]
- Significance of C4d deposition in antibody-mediated rejection. Clin Transplant. 2012;26:43-8.
- [Google Scholar]
- Everolimus inhibits glomerular endothelial cell proliferation and VEGF, but not long-term recovery in experimental thrombotic microangiopathy. Nephrol Dial Transplant. 2006;21:2724-35.
- [Google Scholar]
- Sirolimus-induced thrombotic microangiopathy is associated with decreased expression of vascular endothelial growth factor in kidneys. Am J Transplant. 2005;5:2441-7.
- [Google Scholar]
- Rapamycin impairs recovery from acute renal failure: Role of cell-cycle arrest and apoptosis of tubular cells. Am J Physiol Renal Physiol. 2001;281:F693-706.
- [Google Scholar]






