Translate this page into:
Renal Mucormycosis with Disseminated Lytic Bony Lesions
Corresponding author: Dr. Jasmine Sethi, Post Graduate Institute of Medical Education and Research, Chandigarh, India. E-mail: jasmine227021@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Subramani V, Sethi J, Venkatasubramanian V, Shenoy P, Kundal C, Kumar R, et al. Renal Mucormycosis with Disseminated Lytic Bony Lesions. Indian J Nephrol. 2024;34:270–1. doi: 10.4103/ijn.ijn_308_23
Abstract
Renal Mucormycosis is a lethal opportunistic infection with extensive tissue invasion leading to infarction. We report a diabetic lady with disseminated fungal pyelonephritis presenting with extensive lytic bony lesions mimicking malignancy. Prompt initiation of antifungal therapy and surgical debridement is the key to successful management. A clinician should have a high index of suspicion for Mucormycosis in a patient with non-resolving pyelonephritis and prolonged fever.
Keywords
Mucormycosis
renal
lytic bones
pyelonephritis
fungal
Introduction
Renal and genitourinary mucormycosis are usually seen in immunocompromised individuals and should be suspected in patients of acute pyelonephritis who do not respond to antibiotics. Bony involvement and osteomyelitis caused by mucormycetes is extremely rare. We highlight a patient with fungal pyelonephritis caused by mucormycosis with osteoarticular disseminated lytic lesions. To our knowledge, this is the first reported case of renal mucormycosis with dissemination to bones causing multiple lytic lesions.
Case Report
A woman in her sixth decade with type 2 diabetes presented with a one-month history of fever and weight loss. The patient had a background history of dialysis requiring renal dysfunction, with a previous renal biopsy 2 months back revealing acute interstitial nephritis (AIN) and severe acute tubular injury. Despite the extensive work including autoimmune screen, urine bacterial cultures, urine for acid-fast bacilli/urine gene Xpert, heavy metal screen, serum IgG4 levels, myeloma profile including free light chain assay, and viral markers, the exact etiology remained doubtful. Imaging including a positron emission tomography (PET) was inconclusive apart from mild bulky kidneys. The patient had received steroids for a presumed diagnosis of drug-induced/idiopathic AIN for 3–4 weeks which was stopped later due to poor glycemic control. The serum creatinine had decreased to a nadir of 2–3 mg/dl; however, the patient continued to have intermittent fever, significant weight loss, and worsening malaise.
During the current admission (2 months after the first admission), the patient exhibited neutrophilic leucocytosis with a total count of 15 × 109 per liter with neutrophilic predominance, anemia with hemoglobin of 9.2 gm/dl, blood urea of 140 mg/dl, serum creatinine of 2.7 mg/dl, C-reactive protein of 28 mg/dl, and serum procalcitonin of 7.8 ng/ml. Urinalysis showed pyuria (>30 pus cells/high power field) and culture grew pan-resistant Klebsiella pneumonia. Blood cultures, serum β-D glucan, serum galactomannan, echocardiography, and chest imaging were normal. Repeat PET-CT demonstrated increased fluorodeoxyglucose (FDG) avidity in the bilateral renal cortices with perinephric collections and new lytic lesions involving the sacrum, pelvic bones, vertebrae, ribs, clavicles, and sternum as compared to the previous PET-CT [Figure 1a and b]. Differentials including disseminated malignancy and multiple myeloma were considered in view of extensive lytic lesions. PET-guided biopsy of the sacral lytic lesion and perinephric collection revealed extensive necrotic areas with numerous aseptate fungal hyphae with right-angled branching conforming to mucormycosis [Figure 1c]. The patient was promptly started on liposomal Amphotericin B (5 mg/kg), however, succumbed to septicemia with multi-organ failure one week later.
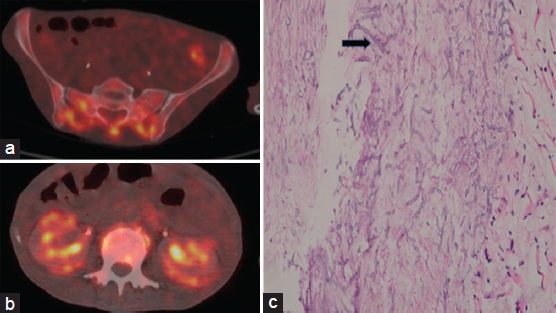
- (a) FDG PET avid lytic skeletal lesions involving the sacrum, pelvic bones, and vertebrae. (b) Bilateral kidneys showing increasing FDG uptake in bilateral renal cortices with FDG-avid perinephric stranding. (c) Biopsy from sacral lesion showing extensive areas of necrosis with numerous broad foldable aseptate hyphae (black arrow) conforming to the morphology of Mucorales (hematoxylin and eosin stain, magnification 40×).
Discussion
Mucormycosis is a lethal opportunistic infection with a predilection for immunocompromised and diabetic patients. The index patient had disseminated mucormycosis (genitourinary, vertebral, bony) with concomitant bacterial pyelonephritis. The risk factors, including uncontrolled diabetes and steroid use, likely contributed to the severity and disseminated nature of the infection. Mucorales is typically angio and tissue invasive, leading to extensive tissue necrosis and infarction.1 Osteoarticular involvement is usually due to hematogenous spread of infection from the primary focus (renal in index patient). Risk factors include hematological malignancies, diabetes mellitus, bone marrow/stem cell transplant, solid organ transplant, and HIV/AIDS. The diagnostic imaging of osteoarticular mucor includes osteolytic lesions, bony destruction/erosion, and MRI bone with T2 weighted signal intensity. Definite diagnoses include biopsy from the involved bony area with culture and histopathology and direct visualization of characteristic ribbon-like hyphae in the clinical specimen.2 There is an increasingly recognized role of FDG PET in the identification of occult invasive fungal disease as well as in doing a guided biopsy.3 Imaging (contrast-enhanced CT) features of renal mucormycosis include patchy/diffuse areas of attenuated contrast enhancement, perinephric fat stranding, bulky psoas muscle, renal abscess, perinephric collection, and thickened Gerota’s fascia.4 Prompt initiation of antifungal therapy, along with aggressive surgical debridement, remains the mainstay of treatment. Our case highlights the need to consider mucormycosis in the differentials of immunocompromised patients with extensive lytic bony lesions. Other differentials of lytic lesions include malignancy with metastasis, multiple myeloma, hyperparathyroidism (brown tumors), giant cell tumor, and Erdheim-Chester disease. This is the first case reported in the literature of renal mucormycosis with multiple lytic lesions involving the entire skeleton.
Conclusion
Renal mucormycosis can have varied presentations including predominantly osteoarticular involvement with lytic lesions mimicking malignancy. A clinician should have a high index of suspicion in an immunocompromised patient with nonresolving pyelonephritis and prolonged fever.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Epidemiology of mucormycosis in India. Microorganisms. 2021;9:523.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Bone and joint infections caused by mucormycetes: A challenging osteoarticular mycosis of the twenty-first century. Med Mycol. 2017;55:691-704.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The role of 18F-fluorodeoxyglucose positron emission tomography/computed tomography (FDG PET/CT) in assessment of complex invasive fungal disease and opportunistic co-infections in patients with acute leukemia prior to allogeneic hematopoietic cell transplant. Transpl Infect Dis. 2021;23:e13547.
- [CrossRef] [PubMed] [Google Scholar]
- Isolated renal mucormycosis in immunocompetent hosts: Clinical spectrum and management approach. Am J Trop Med Hyg. 2019;100:791-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]







