Translate this page into:
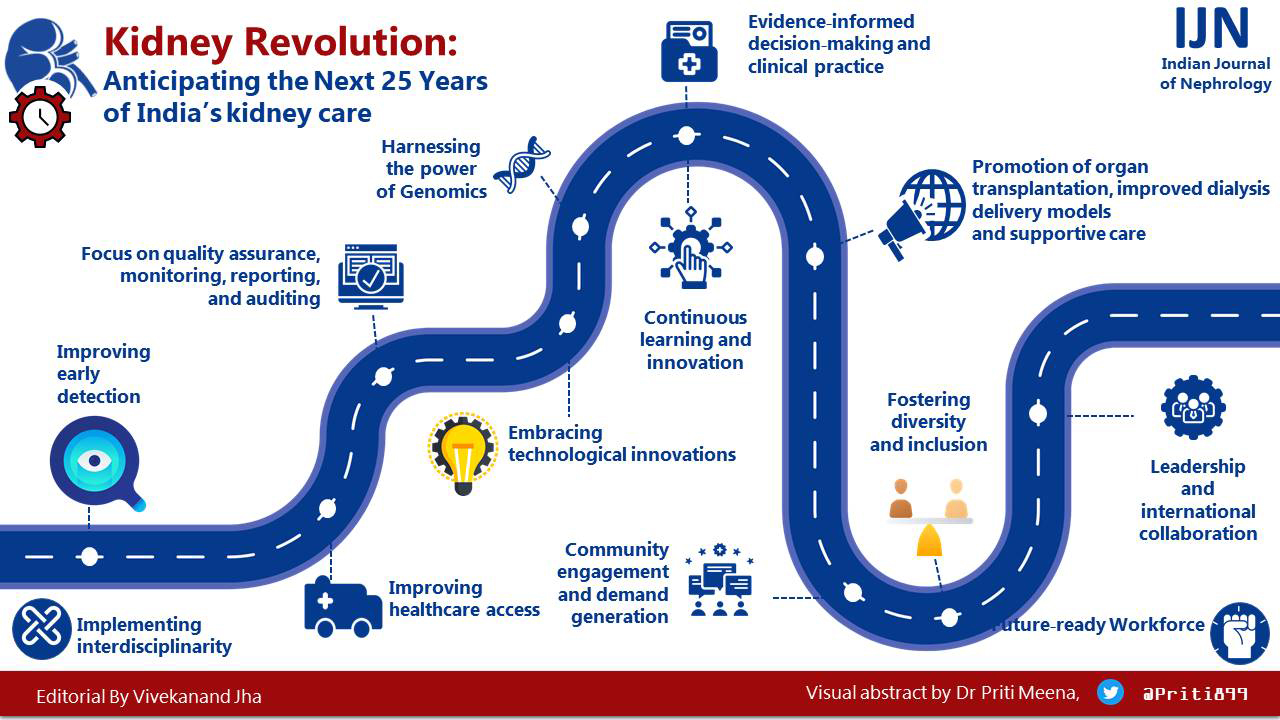
Renal Revolution: Anticipating the Next 25 Years of India’s Kidney Care
Address for correspondence: Prof. Vivekanand Jha, Executive Director, The George Institute for Global Health, 308 Elegance Tower, Jasola Vihar, New Delhi, Delhi - 110 025, India. E-mail: vjha@georgeinstitute.org.in
-
Received: ,
Accepted: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
India will celebrate 100 years of its independence in less than 25 years. Our country has made major gains in healthcare during the last 75 years, particularly in immunization, maternal and child health, and communicable disease control. Article 21 of the Indian Constitution states “No person shall be deprived of his life or personal liberty except according to a procedure established by law,” and it has been interpreted by the Supreme Court to include the right to health and medical care. India is a signatory to the United Nations Sustainable Development Goals.[1] The 2017 National Health Policy aims to ensure access to comprehensive health-care services for all citizens,[2] and the Ayushman Bharat Yojana,[3] announced in 2018, aims to provide financial protection to poor and vulnerable families against catastrophic health-care expenditure.
However, India’s record in improving noncommunicable disease care, the primary cause of premature death and disability in the 21st century, is somewhat mixed. Particularly neglected is the care of patients with and at risk of developing kidney diseases.
Nephrology is a relatively young specialty in India. The Indian Society of Nephrology was established in 1969 and currently has approximately 2600 members. Until recently, kidney care provision was restricted to large cities, but there has been an encouraging increase in access to care in recent years in Tier 2 and 3 cities. However, people living in rural areas are still largely disenfranchised from kidney disease services.
Kidney disease is a significant public health concern in India, with high morbidity and mortality rates. The Million Death Study estimated a 50% increase in deaths due to chronic kidney disease (CKD) between 2001–2003 and 2010–2013.[4] Several surveys have shown a high population prevalence of CKD.[5,6] As many as one out of every five adults in high-prevalence areas has CKD.[7] Similarly, acute kidney injury is common and carries a high mortality, especially because treatment is frequently delayed. However, the National Programme for Prevention & Control of Cancer, Diabetes, Cardio-vascular Diseases and Stroke (NPCDCS), the flagship NCD prevention program in India, does not cover kidney care.
Improving early detection through better understanding of disease burden
There is a need to understand better the burden of kidney disease, including its drivers, to allow the development of adequately targeted screening and early detection programs in different parts of India. We need to understand what drives the high CKD prevalence in some parts of India. In addition to the growing CKD burden secondary to diabetes and hypertension, the contribution of nontraditional risk factors such as maternal malnutrition, exposure to nephrotoxins (e.g. pesticides, heavy metals and some indigenous as well as over the counter medicines) and heat stress, among others, needs to be better understood.[8,9] Anthropogenic climate change and biodiversity loss will likely worsen the kidney disease burden. Disease burden information will help identify at-risk populations to whom early detection programs can be targeted.
Improving access to healthcare
Most of the Indian population lives in rural areas, where access to essential healthcare is limited. There is a severe shortage of kidney health specialists and treatment facilities. This significantly burdens urban centers, leading to overcrowding and long waiting times. Developing resource-sensitive, affordable, scalable, and sustainable models of care requires thinking out of the box – for example, task sharing between nephrologists and nonphysician health-care workers. This approach has already been shown to work for the provision of maternal and neonatal care in India and NCD care in other settings.[10] Online platforms can support the delivery of training to achieve competency and supervision. The need of the populations affected by natural and man-made crises should be kept in mind.
Community engagement and demand generation
The lack of awareness about kidney disease in public and among health-care professionals is a significant challenge. A comprehensive approach to addressing this requires community engagement, awareness raising, advocacy campaigns (as during World Kidney Day),[11] reforms in medical curricula, and collaborations between nephrology societies and other professional groups. This will raise the demand for diagnostic facilities, essential preventive treatment, and overall improvement in service quality.
The neglect of kidney diseases in undergraduate and postgraduate medical curricula needs to be remedied. It is surprising to note the gap in policy announcements, awareness, and implementation. For example, the Government of India announced the guidelines for implementing the peritoneal dialysis program[12] under the National Health Mission and, later, One Nation, One Dialysis program in 2019. Even though this program has the potential to expand the reach of dialysis and reduce inequities, large sections of the Indian kidney care community remain unaware of its existence and how it is to be implemented. In the meantime, tens of thousands of patients are dying for want of dialysis. This knowledge-implementation gap needs to close.
Promotion of organ transplantation, improved dialysis delivery models and supportive care
Indian subjects with kidney failure are significantly younger than their Western counterparts, raising the imperative for strengthening kidney transplant services. The high cost of care and the shortage of organs for transplantation are significant challenges. Our of all kidney replacement services, transplantation provides the highest value for money, and needs to be publicly funded. Notably, some states do have government-funded transplantation programs Institution-level barriers and lack of coordination discourage organ donation. National and regional networks should promote the efficiency and coordination of deceased organ donation. Regulations should remove disincentives from donations by altruistic living kidney donors and punish illegal commercial transplants.
We need to innovate with regard to dialysis delivery. The National Dialysis Program has sunstantially reduced the barrier to access and led to rapid increase in the uptake of hemodialysis services, but the outcomes still remain sub-optimal. Better business models need to be built that leverage the efficiencies of large dialysis organizations. The shortage of dialysis professionals in remote areas can be addressed through a network approach in which established ‘hub’ units support a number of ‘spoke’ units. Jobs should be defined in terms of competencies and not specific roles (for example, a doctor, as well as a trained nurse, can place dialysis catheters). The power of PD needs to be harnessed by developing a network model, and promotion of assisted PD (paid if required), in which a trained health worker assists in preforming PD for those who require support, under regional guidance.
Dialysis needs to become environmentally sustainable. Models of care are being developed in many countries and Indian community can adopt and adapt many of them.
There is a need to promote supportive kidney care[13] that focuses on addressing the holistic needs of patients with advanced kidney disease, including their physical, psychological, social, and spiritual needs. Supportive care is sometimes thought of as “no care,” but it is time to dispel that myth. Supportive care involves understanding the values and preferences of the patients, addressing their medical and nonmedical needs, such as symptom management, social support, financial assistance, and psychological counseling, and involving patients in their care and treatment decisions.
Focus on quality assurance, monitoring, reporting, and auditing
Anything that is not measured does not get done. The quality assurance, monitoring, and reporting culture is lacking in the kidney care community in India. Continuous quality improvement involves setting goals, collecting and analyzing data, implementing changes, and measuring and reporting outcomes. Kidney professionals should develop quality measures around clinical outcomes, patient experience, and health-care utilization. Better implementation of electronic health records, disease registries, and audits will help assess adherence to quality measures and help identify improvement areas. Quality matrics should be evidence based, relevant to patient outcomes, and feasible to measure. The standards for dialysis quality have already been developed by Indian Society of Nephrology. Minimum quality standards need to be set for all dialysis programmes, regularly monitored, audited and payments in the National dialysis programme be given according to the quality parameters achieved.
Evidence-informed decision-making and clinical practice
It is time that kidney care professionals in India use the best available scientific evidence to guide decision-making and decide treatment approaches for patients with kidney diseases. Evidence-informed policies and guidelines for kidney health management will lead to a more standardized and effective approach to care for patients with kidney disease. This will reduce variations in care and low-value care, improve patient outcomes, and increase cost-effectiveness. Implementation will require a mix of incentives, including education, policy reforms, developing, disseminating and implementing the use of evidence-based guidelines, involving patients in decision-making and promoting a culture of continuous learning and improvement. Development of Standard Treatment Workflows for management of common conditions at different healthcare levels by the Department of Health Research, and recent guideline development initiatives by the kidney care are steps in the right direction.
Implementing interdisciplinarity
Kidney diseases and their consequences present complex problems. Kidney disease hardly ever develops in isolation. There is overwhelming evidence that embracing interdisciplinarity can improve the quality of care and outcomes and allow more effective use of resources. Interdisciplinarity allows the development of a comprehensive approach to understand a patient’s condition and to design more effective treatment plans; it also helps in better problem-solving through more innovative and effective solutions, streamlined processes, and reduced duplication of effort, leading to more efficient use of time and resources and helping understand complex diseases or conditions. Multidisciplinary care is more patient centered, holistic, and cost-effective.
Embracing technological innovations
Technological advancements in kidney care delivery can enhance the quality of care provided to patients, improve outcomes, and reduce health-care costs. The Indian clinical and research community should anticipate advancements in telemedicine, wearables, remote monitoring technologies, artificial intelligence, and biomarker science. Policymakers can utilize advancements in data analytics to identify gaps in kidney care delivery, evaluate the effectiveness of existing programs, and develop evidence-based policies. Improvements in interoperability can improve the exchange of health information between health-care providers, enhancing the quality of care provided to patients with kidney disease. The funder community needs to support health-care innovation financing. Use of big data approaches and database linkages will allow an easier pathway to personalized medicine (e.g. by more accurate risk-stratification), quality improvement (e.g. by identifying and minimizing variations in clinical practice) and public health surveillance (e.g. tracking disease burden and success of programs). Big data can also help with better design of clinical trials.
Harnessing the power of genomics
Understanding an individual’s genetic makeup can help improve our ability to offer personalized treatment (e.g., avoiding toxic immunosuppressive therapy in an individual with focal semental glomerulosclerosis due to a genetic cause); it can also help in risk stratification, predictive testing (for example, the likelihood of recurrence of hemolytic uremic syndrome after kidney transplantation), family screening (e.g., to identify those at risk of developing a genetic disease or to identify a kidney donor) and antenatal counselling. With a population of 1.4 billion, the possibility of genetic diversity in India are immense. A national repository of genetic data can facilitate improved diagnosis and research by identifying local variations and their associations with diseases.
Contribute to evidence generation
In addition to being consumers, the Indian nephrology community needs to take on a more active role in evidence generation and contribute to the global knowledge base through more high quality basic science, clinical, translational and implementation research. Such research will help address local health challenges, develop evidence-based guidelines and policies critical for improving healthcare delivery and outcomes, and enhance research capacity through building better research infrastructure, skills and knowledge, and facilitating collaborations.
Continuous learning and innovation
The Indian kidney health community should be prepared for tomorrow and anticipate advancements in digital health, artificial intelligence, machine learning,[14] precision medicine, and regenerative medicine. Digital health can better inform risk stratification, population health, and preventive care (in combination with task sharing) and improve patient engagement and self-management, leading to better health outcomes for patients with kidney disease.
Precision medicine can help tailor treatments to individual patients, improving treatment effectiveness and reducing health-care costs. Regenerative medicine, on the other hand, can help repair damaged kidney tissues and improve kidney function. Artificial intelligence and machine learning algorithms can analyze large volumes of data and help make more accurate diagnoses, predict diseases, and develop bespoke treatment plans based on individual patient needs.
Other technologies like nanotechnology (by enabling targeted drug delivery and through the development of more efficient medical devices), 3-D printing (for surgical planning, developing kidney models for drug testing, and eventually bioprinting functional kidneys from the patient’s cells), technologies using gene editing like CRISPR-Cas9 (to treat genetic diseases by targeting and modifying specific genes responsible for diseases), and virtual and augmented reality (to create immersive training and simulation experiences for medical professionals and patients) hold immense potential.
Future-ready workforce
The Indian kidney care community needs to develop a multidisciplinary workforce ready to use future technologies and provide high-quality care to patients. This involves identifying the needed skills and competencies, incorporating technology into education and training at all levels, ongoing professional development through multidisciplinary collaboration and innovation, and promoting a culture of continuous learning. The latter requires mentorship programs, career development plans, and recognition for those who demonstrate a commitment to learning and innovation.
Fostering diversity and inclusion
Indian kidney care community must ensure its commitment to equity and eradication of prevalent injustices. A diverse health-care workforce better understands and can respect the differences in our societies and provide quality care that meets each patient’s needs. This can reduce disparity, increase the comfort and trust in the patient community, and improve creativity, culminating in a more robust health-care workforce.
Leadership and international collaboration
We live in a globalized world. A global outlook and collaboration help improve clinical care through knowledge sharing, resource pooling, improved efficiency, standardization of care, and improved research, resulting in improved quality of care and outcomes. Global collaboration facilitates advocacy to promote greater investment in research, policy change, and education. Indian nephrology training has long been recognized to be excellent, has made significant strides over the last quarter century, can and should provide leadership to help develop kidney care in the immediate neighbourhood and other countries in similar socioeconomic situations.
A quarter century ago, it would have been impossible to predict that we would be in the current situation. Although the challenges appear daunting, we have numerous tools at our disposal. This requires, however, a concerted effort on the part of the clinical, research, policymaker, and funder community to ensure a future in which all Indians have access to high-quality kidney care.
References
- Sustainable development, goals. Available from:https://www.globalgoals.org/goals/
- National Health Policy 2017. Available from:https://www.nhp.gov.in/nhpfiles/national_health_policy_2017.pdf
- Ayushman Bharat. Available from:https://ab-hwc.nhp.gov.in/
- Renal failure deaths and their risk factors in India. 2001-13:Nationally representative estimates from the Million death study. Lancet Glob Health. 2017;5:e89-95.
- [Google Scholar]
- Prevalence of early stages of chronic kidney disease in apparently healthy central government employees in India. Nephrol Dial Transplant. 2010;25:3011-7.
- [Google Scholar]
- Prevalence of low glomerular filtration rate, proteinuria and associated risk factors in North India using Cockcroft-Gault and Modification of Diet in Renal Disease equation:An observational, cross-sectional study. BMC Nephrol. 2009;10:4.
- [Google Scholar]
- A systematic study of the prevalence and risk factors of CKD in Uddanam, India. Kidney Int Rep. 2020;5:2246-55.
- [Google Scholar]
- Chronic kidney disease of unknown etiology in India:What do we know and where we need to go. Kidney Int Rep. 2021;6:2743-51.
- [Google Scholar]
- Climate change and the emergent epidemic of CKD from heat stress in rural communities:The case for heat stress nephropathy. Clin J Am Soc Nephrol. 2016;11:1472-83.
- [Google Scholar]
- Cardiovascular disease risk factor prevalence and estimated 10-year cardiovascular risk scores in Indonesia:The SMARThealth extend study. PLoS One. 2019;14:e0215219.
- [Google Scholar]
- Available from:https://www.worldkidneyday.org/
- GUIDELINES FOR ESTABLISHING PERITONEAL DIALYSIS SERVICES. Available from:https://nhm.gov.in/New_Updates_2018/PMNDP/Guidelines_for_PMNDP.pdf
- Availability, accessibility, and quality of conservative kidney management worldwide. Clin J Am Soc Nephrol. 2020;16:79-87.
- [Google Scholar]
- Artificial intelligence-enabled decision support in nephrology. Nat Rev Nephrol. 2022;18:452-65.
- [Google Scholar]






