Translate this page into:
The role of neutrophil-gelatinase-associated lipocalin in early diagnosis of contrast nephropathy
Address for correspondence: Dr. M. R. Khatami, Nephrology Research Center, Imam Khomeini Hospital, Keshavarz Blvd, 1419733141, Tehran, Iran. E-mail: khatamis@sina.tums.ac.ir
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Neutrophil-gelatinase-associated lipocalin (NGAL) is a biomarker of acute kidney injury. The aim of this study was to define a cut-off for NGAL in the early diagnosis of contrast-induced nephropathy (CIN) in patients with normal kidney function. We enrolled 121 patients with normal serum creatinine who underwent coronary angiography. NGAL was measured in urine before the procedure and 12 and 24 h afterward. CIN was defined as a 0.3 mg/dl increase in serum creatinine within 48 h after the procedure. Seven of 121 patients had CIN (5.8%). The NGAL levels in the 12- and 24-h urine samples of these patients were 30 (5–45) and 20 (15–40) ng/ml, respectively, whereas those in patients without CIN were 15 (5–45) and 15 (10–51) ng/ml, respectively (P = 0.8). In patients with CIN, the sensitivity and specificity of NGAL with a cut-off of 22.5 ng/ml were 71.4% and 57.9% in 12-h urine samples, with the negative predictive values (NPV) and positive predictive values (PPV) of 97.1% and 9.4%, respectively. In conclusion, we suggest that urine NGAL with cut-off point of 22.5 ng/ml has acceptable sensitivity and specificity for early diagnosis of CIN in patients with normal serum creatinine, but regarding NPV and PPV the best performance of this value is to rule out the CIN in patients at risk who received contrast media.
Keywords
Acute kidney injury
contrast nephropathy
coronary angiography
neutrophil-gelatinase-associated lipocalin
serum creatinine
Introduction
Contrast-induced nephropathy (CIN) is the third leading cause of acute kidney injury (AKI) in hospitalized patients. It is associated with significant morbidity and mortality.[12] As a result of extensive use of contrast agents, the burden of this complication is increasing.[3] The incidence of CIN is reported to be 0.6–2.3% among the general population who have no risk factors for CIN, but as high as 90% among high-risk patients.[45] Aside from major advances in the pathophysiology of the disease, prevention is the only way to control the complications of this disorder.
Among the various causes of AKI, contrast nephropathy is unique because the exact timing of exposure to the nephrotoxin is known. Therefore, a step-by-step evaluation of the biological and structural changes in the kidney can be performed. Biomarkers that can detect very early injuries may improve the management of the disease, as well as increase our understanding of the pathophysiology of this disorder. Traditionally, CIN has been defined as a relative increase of 25% and/or an absolute increase of 0.5 mg/dl in serum creatinine. But based on Kidney Disease: Improving Global Outcomes, CIN was defined as increase in serum creatinine by 0.3 mg/dl within 48 h.[6] However, serum creatinine is an unreliable indicator of acute changes in renal function.[7] Several studies have evaluated the roles of various biomarkers in the early diagnosis of AKI in critically ill patients. Neutrophil-gelatinase-associated lipocalin (NGAL) has been introduced as a new biomarker for early detection of acute renal failure.[89] NGAL is a small protein that is expressed on the surface of neutrophils and epithelial cells, such as renal tubule cells, and may be over-expressed in ischemic and toxic kidney injuries. NGAL is present in plasma and urine; it can be detected in plasma and urine from AKI patients only 2 h after kidney injury.[10] Since its introduction, few studies have evaluated the role of NGAL as a diagnostic marker for CIN.[1112131415] The aim of our research was to define a NGAL cut-off for the early diagnosis of CIN in patients with normal serum creatinine who develop CIN following coronary angiography.
Methods
In this process evaluation study, we enrolled 121 patients referred for coronary angiography. The study was approved by the Deputy Research Ethics Board of Tehran University of Medical Sciences. All patients were over 18 years old with serum creatinine levels in the normal range (male ≤1.5 mg/dl, female ≤1.3 mg/dl). Patients with a previous history of chronic kidney disease or abnormal urinalysis results were excluded. We also excluded patients who had received nephrotoxin agents including contrast media during the week before angiography. All hemodynamically unstable patients and patients undergoing emergent angiography were also excluded. The eligible patients were recruited sequentially by convenience sampling until the sample size was completed. After enrolment, patients who had other causes of AKI, needed to use nephrotoxin agents, were re-exposed to contrast media, or had surgery before completing the study were excluded. All patients received 0.9% saline infusion (1 ml/kg body weight) starting at 4 h before the procedure and continuing for 8 h after angiography. Diuretics were discontinued from 24 h before procedure until 24 h after angiography. Iodixanol, an iso-osmolar contrast media was used in all patients. The volume of contrast was calculated as weight × 5/serum creatinine. Blood and timed urine samples were collected at specified intervals. Urine samples (5 ml) were obtained at 0, 12 and 24 h. The urine samples were centrifuged and stored at −84°C. Urinary NGAL was measured by the monoclonal enzyme-linked immunosorbent assay (ELISA) sandwich method using commercially available kits (Human NGAL Rapid ELISA Kit [KIT 037], Bioporto Diagnostic Company, Denmark).
CIN was defined as an increase of 0.3 mg in serum creatinine within 48 h after contrast exposure.
Statistical analysis
Analysis of data was performed using Statistical Package for the Social Sciences version 18 (SPSS, Chicago, IL, USA). The distribution of continuous variables was examined by the Kolmogorov-Smirnov test. The Wilcoxon signed-rank test was then used to compare the two related continuous variables. Repeated measurement analysis was used to compare the means of urinary NGAL for three measurements between groups. To evaluate the cut-off of urine NGAL for predicting CIN after angiography and its sensitivity and specificity, we used receiver-operating characteristic curve (ROC) analysis; the cut-off value was estimated using the Youden index, the maximum difference between sensitivity (true positive) and 1-specificity (false positive). Continuous variables were presented as means ± standard deviation or medians (inter-quartile range). P < 0.05 was deemed to indicate statistical significance.
Results
The characteristic data of all patients are shown in Table 1. There was no difference in CIN development between males and females (P = 0.2). Seven patients (5.8%) had CIN.

We found no significant differences in baseline creatinine, body mass index and contrast volume in patients with and without CIN. The age was significantly lower in CIN group (P = 0.015). The base urine NGALs were 5 (5–15) ng/ml and 6.9 (5–15) ng/ml in patients with and without CIN, respectively (P = 0.7). In patients without CIN, the NGALs in 12- and 24-h urine samples were 15 (5–45) ng/ml and 15 (10–51) ng/ml, respectively, whereas in CIN patients the values were 30 (5–45) ng/ml and 20 (15–45) ng/ml, respectively (P = 0.8). All results of timed point urine NGAL are shown in Table 2.
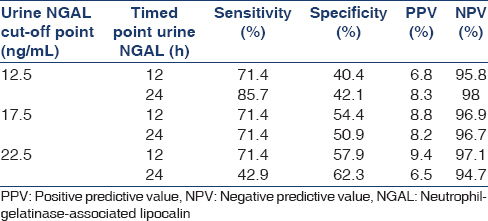
The accuracy of using urine NGAL in the diagnosis of CIN is depicted in Figure 1.
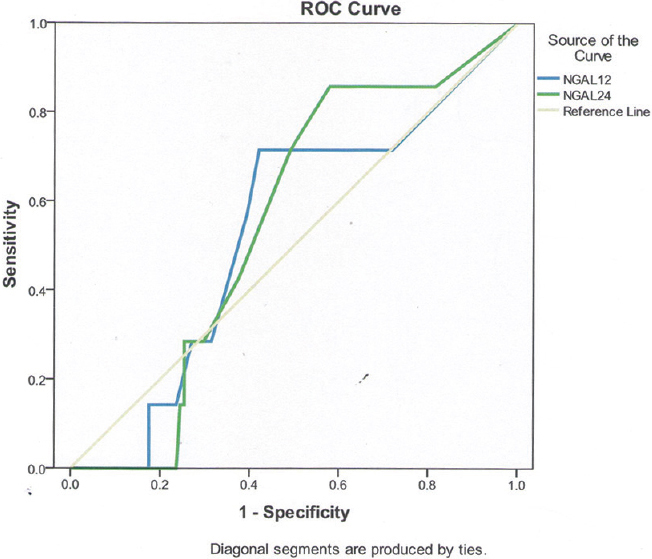
- Accuracy of urine neutrophil-gelatinase-associated lipocalin in diagnosis of contrast-induced nephropathy
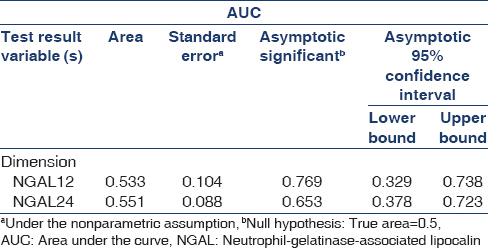
The area under the curve for NGAL in 12 and 24-h urine samples from patients with CIN is presented in Table 3.
Discussion
In the current study, 37% of the patients had CIN as defined by a 25% increase in base serum creatinine, whereas only 5.8% of the patients were diagnosed with CIN 0.3, which is in concordance with most reports in literature.[161718] The prevalence of CIN has been reported to be 0–50%.[19] This highly variable prevalence is due to differences in age, sex, associated diseases, etc., among patients, and in medical procedures, such as the volume and route of contrast agent administration among studies. In our study, when we considered the absolute increase in serum creatinine, the prevalence of CIN was similar to that of other studies. However, the prevalence of CIN according to the relative increase in serum creatinine was surprisingly high. This wide variation in the incidence of CIN in our patients may be explained by “hospital-induced nephropathy.” It has been shown that significant changes in serum creatinine may occur from day to day in hospitalized patients who have not been exposed to contrast agents. Interestingly, depending on the definition of CIN used, this variation was found to be 5–35% even in patients who did not receive any contrast agents.[20] It is possible that this phenomenon was more pronounced in our patients, because even slight changes in serum creatinine may cause a 25% relative increase in serum creatinine while the absolute increase may be <0.3 mg/dl. So, creatinine is an insensitive and delayed marker of early changes in kidney function.[212223] Biomarkers are known as a marker of kidney damage whereas serum creatinine and urine output are determinants of kidney function. There may be discrepancy between these two markers in AKI. Potential changes in biomarkers should be considered regarding the hydration status and diuretic therapy. Intravenous diuretic therapy may be accompanied by tubular damage in some patients, as assessed by a rise in urine NGAL.
So it is very important to define the exact value of each in different settings of AKI. More studies are needed to clarify the exact values of threshold, sensitivity, specificity, positive predictive values (PPV) and negative predictive values (NPV) of each biomarker in different conditions of AKI.[24] Our study is a step to unveil the value of urine NGAL in AKI due to CIN.
Among several biomarkers used for the early diagnosis of AKI, NGAL is effective.[10] Mishra first introduced this biomarker for the early diagnosis of acute renal failure.[8] Since then, many clinical trials have been conducted, most of which were of high-risk AKI patients.[925262728] To date, there has been no evaluation of the cut-off values for NGAL in patients with CIN, although some studies have reported NGAL cut-off values in critically ill patients. For instance, studies on children in the intensive care unit or who underwent cardio-pulmonary surgery reported that a cut-off of 50–100 ng/ml showed a sensitivity of 80–100% and specificity of 90–100%.[925] Additional studies in critically ill adult patients reported that higher NGAL cut-off values (130–250 ng/ml) showed 73–90% sensitivity and 78–99% specificity for predicting an early AKI diagnosis.[262728] It is not surprising that the NGAL cut-off values in our study are much lower than those reported previously, because our patients were in a stable condition, in contrast to the critically ill patients in other studies who had major and multiple risk factors for AKI. Few studies have examined the role of NGAL in the early diagnosis of CIN.[1112131415] All examined a limited number of cases (35–100 patients). A study by Bachorzewska-Gajewska et al.[13] showed that when CIN was defined as a 25% increase in serum creatinine or serum cystatin C levels sensitivity was 90% and specificity was 74%, while Hirsch et al. found that an increase in urinary NGAL levels showed 76% sensitivity and 80% specificity;[14] using a cutoff value of 100 ng/ml, sensitivity, specificity, and area under the ROC curve for prediction of CIN were excellent for the 2-h urine NGAL (73%, 100%, and 0.92, respectively). Another study included patients with decreased glomerular filtration rate (GFR),[15] and two other studies reported no changes in serum creatinine before and after contrast exposure.[1112] In McCullough et al., 2 of 63 patients with GFR <75 ml/min showed increased serum creatinine[15] One study indicated that a 25% increase in urine NGAL showed sensitivity and specificity of 80% and 83%, respectively within 8 h of contrast administration.[29]
The advantage of using urinary NGAL over serum NGAL is that urinary NGAL likely indicates local kidney injuries and is a non-invasive method. Nevertheless, urine proteins may interfere with NGAL measurement.[25]
We compared levels of urinary NGAL at various time points to determine the optimum cut-off and time point for accurate early diagnosis of CIN. Although the sensitivity of cut-off point of 12.5 ng/ml was the highest among all values (85.7%), but its lowest specificity and its performance in 24 h urine sample makes it inferior for purpose of early diagnosis of CIN. Meanwhile, the cut-off point of 22.5 ng/ml in 12 h urine sample seems to have the best performance with the sensitivity of 71.4% and specificity of 57.9% the NPV and PPV of this cut-off point was 97.1% and 9.4%, respectively. The difference in the specificity of urine NGAL in our study in comparison with other reports can be explained by differences in the definitions of AKI and different AKI settings.
Our study showed that the PPV of these values of NGAL is low but the NPV is very high. It may suggest that urine NGAL in range of 12.5–22.5 ng/ml has a power to rule out the CIN early.
The limitations of the current study were that the NGAL measurements were performed in urine samples only, not earlier than 12 h. The strength of this study was the number of patients, which represented the largest sample size of similar studies to date; we also included patients with normal serum creatinine, whereas other studies examined patients with different stages of renal function. The other advantage of our study was that we determined a cut-off value of NGAL for early diagnosis of CIN, which has to our knowledge not been reported previously.
Conclusion
A urinary NGAL cut-off point of as little as 12.5 ng/ml has acceptable sensitivity and specificity for early diagnosis of CIN, while the best performance is with the value of 22.5 ng/ml at 12 h urine sample. But regarding to predictive value of these measures, we showed clearly that the urine NGAL <12.5 ng/ml is an excellent tool to rule out the CIN in patients with normal serum creatinine.
Source of Support: A grant by research deputy of Tehran University of Medical Sciences
Conflict of Interest: None declared.
References
- Contrast-induced nephropathy: Clinical insights and practical guidance-a report from the cin consensus working panel-overview. Am J Cardiol. 2006;98:2K-4.
- [Google Scholar]
- The clinical and renal consequences of contrast-induced nephropathy. Nephrol Dial Transplant. 2006;21:i2-10.
- [Google Scholar]
- Contrast-induced nephropathy in patients undergoing primary angioplasty for acute myocardial infarction. J Am Coll Cardiol. 2004;44:1780-5.
- [Google Scholar]
- Epidemiology and prognostic implications of contrast-induced nephropathy. Am J Cardiol. 2006;98:5K-13.
- [Google Scholar]
- Risk factors and therapy strategies for contrast-induced nephropathy. Ren Fail. 2006;28:365-81.
- [Google Scholar]
- Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2:1-138.
- [Google Scholar]
- Defining acute renal failure: Physiological principles. Intensive Care Med. 2004;30:33-7.
- [Google Scholar]
- Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. J Am Soc Nephrol. 2003;14:2534-43.
- [Google Scholar]
- Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet. 2005;365:1231-8.
- [Google Scholar]
- NGAL: An emerging biomarker of acute kidney injury. Int J Artif Organs. 2008;31:199-200.
- [Google Scholar]
- Could neutrophil-gelatinase-associated lipocalin and cystatin C predict the development of contrast-induced nephropathy after percutaneous coronary interventions in patients with stable angina and normal serum creatinine values? Kidney Blood Press Res. 2007;30:408-15.
- [Google Scholar]
- Neutrophil-gelatinase-associated lipocalin and renal function after percutaneous coronary interventions. Am J Nephrol. 2006;26:287-92.
- [Google Scholar]
- NGAL (neutrophil gelatinase-associated lipocalin) and cystatin C: Are they good predictors of contrast nephropathy after percutaneous coronary interventions in patients with stable angina and normal serum creatinine? Int J Cardiol. 2008;127:290-1.
- [Google Scholar]
- NGAL is an early predictive biomarker of contrast-induced nephropathy in children. Pediatr Nephrol. 2007;22:2089-95.
- [Google Scholar]
- Neutrophil gelatinase-associated lipocalin: A novel marker of contrast nephropathy risk. Am J Nephrol. 2012;35:509-14.
- [Google Scholar]
- Impact of gender on the incidence and outcome of contrast-induced nephropathy after percutaneous coronary intervention. J Invasive Cardiol. 2003;15:18-22.
- [Google Scholar]
- Acute renal failure after coronary intervention: Incidence, risk factors, and relationship to mortality. Am J Med. 1997;103:368-75.
- [Google Scholar]
- Contrast-induced nephropathy: Contrast material not required? AJR Am J Roentgenol. 2008;191:383-6.
- [Google Scholar]
- Estimation of glomerular filtration rate in patients with normal serum creatinine undergoing primary PCI: Is it really normal? Nephrol Dial Transplant. 2006;21:1736-8.
- [Google Scholar]
- Urine NGAL predicts severity of acute kidney injury after cardiac surgery: A prospective study. Clin J Am Soc Nephrol. 2008;3:665-73.
- [Google Scholar]
- Potential use of biomarkers in acute kidney injury: Report and summary of recommendations from the 10 th Acute Dialysis Quality Initiative consensus conference. Kidney Int. 2014;85:513-21.
- [Google Scholar]
- Urinary neutrophil gelatinase-associated lipocalin and acute kidney injury after cardiac surgery. Am J Kidney Dis. 2008;52:425-33.
- [Google Scholar]
- Sensitivity and specificity of a single emergency department measurement of urinary neutrophil gelatinase-associated lipocalin for diagnosing acute kidney injury. Ann Intern Med. 2008;148:810-9.
- [Google Scholar]
- Urine neutrophil gelatinase-associated lipocalin and interleukin-18 predict acute kidney injury after cardiac surgery. Ren Fail. 2008;30:904-13.
- [Google Scholar]
- Neutrophil gelatinase-associated lipocalin (NGAL) correlations with cystatin C, serum creatinine and eGFR in patients with normal serum creatinine undergoing coronary angiography. Nephrol Dial Transplant. 2007;22:295-6.
- [Google Scholar]
- Can neutrophil gelatinase-associated lipocalin help depict early contrast material-induced nephropathy? Radiology. 2013;267:86-93.
- [Google Scholar]







