Translate this page into:
Tuberculosis in Hemodialysis: Catch me if you can
Address for correspondence: Dr. Mohammed Asserraji, Nephrology Unit, Avicenne Military Hospital, Marrakesh - 40000, Morocco. E-mail: asserrajimed@hotmail.com
-
Received: ,
Accepted: ,
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Among chronic kidney disease (CKD) population, the risk of active tuberculosis (TB) is increased, especially in low and middle income countries (LMICs).[1] Several publications have shown TB as an important source of morbidity and mortality in dialysis patients.[2] Factors such as urémia, poor nutritional status, vitamin D deficiency, and hyperparathyroidism contribute to immunodeficiency and increase the risk of TB in CKD patients.[3] Clinical presentation of TB in CKD patients is usually insidious and atypical.[12] In this context, we report a very uncommon case of pancreatic TB in a CKD patient who had been confused with pancreatitis on imaging. Macroscopic and histopathological finding after laparotomy performed for suspicion of pancreatic malignancy showed granuloma. Interferon-gamma release assays (IGRAs) by Quantiferon-Gold assay were positive. Anti-tuberculous therapy (ATT) was initiated with complete resolution of symptoms.
A 62-year-old male with end-stage renal disease (ESRD) was referred for abdominal pain, vomiting, weight loss, and persistent fever (>39°C). ESRD was secondary to hypertension. He had been on hemodialysis (HD) three times a week for almost 7 years and was completely anuric. BCG vaccination status was unclear. Renal replacement therapy by HD showed no particular issues. Onfirst examination, the patient was very tired with fever 38.5°C, normal blood pressure, and epigastric tenderness. The fistula exam was normal. Biochemical tests revealed azotemia (serum creatinine 5.4 mg/dl, urea 1.2 g/l), C-reactive protein 171 mg/l, procalcitonine 1.420 ng/ml, hemoglobin 9.1 g/dl, serum ferritin 284 ng/ml, and intact parathyroid hormone 216 ng/l. Human immunodeficiency virus (HIV) status was negative. Pancreatic enzyme was slightly increased (hyperlipasemia 95 U/l and hyperamylasemia 224 U/l). The chest radiography was normal and computed tomogram (CT) scan abdomen revealed enlarged edematous pancreas, which was initially thought to be acute pancreatitis (Balthazar grade C) associated with multiples mesenteric and aortocaval lymph nodes [Figure 1]. This pattern is more related to an inflammatory process rather than malignant infiltration. Since no clear etiology of pancreatitis with nodes had been found so far, laparotomic exploration was then performed for histopathological examination. Cytology demonstrated granuloma, an organized immunological structure including macrophages, monocytes, dendritic cells, neutrophils, epithelioid cells, and multi-nucleated giant cells [Figure 2]. Acid-fast bacilli (AFB) culture was negative and quantiferon-Gold assay was positive. Real-time PCR (polymerase chain reaction) for the detection of Mycobacterium was unavailable. Anti-tuberculous therapy (ATT) was initiated for 6 months with the complete resolution of symptoms.

- Computed tomogram (CT) scan showing enlarged edematous body of pancreas (Balthazar grade C)
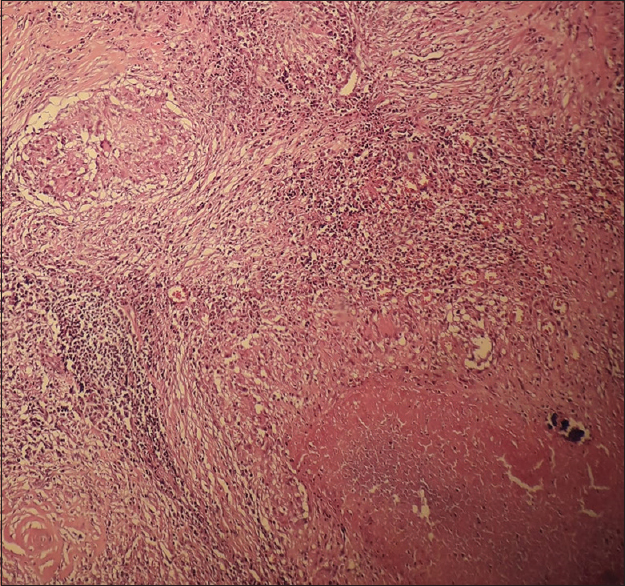
- Granulomatous inflammation with epitheloid cells, and lymphocytes
TB remains a common cause of infectious morbidity and mortality worldwide.[1] However, the pancreatic localization of this condition is extremely rare and can be confused, on imaging, with malignancy or pancreatitis.[12] The clinical presentation of pancreatic TB is not specific and includes weight loss, anorexia, abdominal pain, fever, night sweats, back pain, and jaundice. Patients with pancreatic TB present with several common pancreatic diseases such as acute pancreatitis, pancreatic neoplasm, pancreatic cyst, or an abscess, etc.
Several reports showed a strong link between CKD and active TB. CKD patients are 3 to 25 times more likely to suffer from TB than the general population. Furthermore, these patients, once exposed to TB, present high rates of atypical clinical presentations and mortality.[1] Country of birth represents an important TB risk factor in dialysis populations. Among some low-income countries, TB incidence can reach 698 per 100,000 per year supporting the hypothesis that active TB results more from reactivation of latent TB infection (LTBI) acquired before dialysis initiation than from recent exposure and infection. Once exposed to TB infection, dialysis patients do represent an additional risk to other patients and health care workers in hemodialysis units. This is to underline the importance of appropriate screening and active TB case detection in order to prevent TB transmission inside dialysis units.[1]
There are no authentic radiological aspects of pancreatic TB and most cases have been recognized after laparotomy performed for suspicious malignancy.[4] Immune assays and histopathology are the cornerstone of TB infection detection.[12] The tuberculin skin test (TST) is limited by high percentages of both false-negative. Interferon-gamma release assays (IGRAs) is more promising for TB diagnosis in this setting. Nevertheless, both TST and IGRAs have been shown with poor predictive value for active TB in advanced CKD patients.[12]
In conclusion, both epidemiological trends of TB and CKD are rising.[35] These two conditions are closely related to poor countries.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Tuberculosis and chronic kidney disease: An emerging global syndemic. Kidney Int. 2016;90:34-40.
- [Google Scholar]
- Chronic kidney disease: Global dimension and perspectives. Lancet. 2013;382:260-72.
- [Google Scholar]
- Diagnosis of tuberculosis in dialysis patients: Current strategy. Clin J Am Soc Nephrol. 2010;5:1114-22.
- [Google Scholar]
- Risk of tuberculosis in dialysis patients: A nationwide cohort study. PLoS One. 2011;6:e29563.
- [Google Scholar]






