Translate this page into:
Tunneled Hemodialysis Catheter Making Its Way into the Spinal Canal: An Unusual Complication
Corresponding author: Vinay Rathore, Department of Nephrology, All India Institute of Medical Sciences, Raipur, Tatibandh, Chhattisgarh, India. E-mail: vinayrathoremd@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Saha AK, Bodhey NK, Kashyap NK, Rathore V, Badge RP, Aggarwal J, et al. Tunneled Hemodialysis Catheter Making Its Way into the Spinal Canal: An Unusual Complication. Indian J Nephrol. doi: 10.25259/IJN_53_2024.
Abstract
The procedure of tunnelled hemodialysis catheter insertion is generally considered safe. We report the case of a lady who had a malpositioned femoral tunneled hemodialysis catheter that entered into the spinal canal causing neurological weakness. The catheter was later safely removed leading to partial neurological recovery.
Keywords
Tunneled hemodialysis catheter
Malposition
Spinal canal
Neurological weakness
Interventional nephrology
Introduction
Tunneled hemodialysis (HD) catheters are commonly used for vascular access as a bridge till the maturation of an arterio-venous fistula (AVF).1
HD catheter insertion is occasionally complicated by bleeding, hematoma, pleural puncture, air embolism, and malpositions.2 Malposition of a catheter into the spinal cord has never been encountered. We report a case of such a malposition and the management strategy to remove the same.
Case Report
A 52-year-old female who had a known case of chronic kidney disease and had been on maintenance HD (MHD) for the last 2 months. She visited our outpatient department with poor blood flow through the right IJV nontunneled HD catheter.
She was diagnosed as a case of diabetic kidney disease 2 years back, initially managed conservatively, and later initiated on MHD for uremic symptoms. Dialysis was initiated through a right IJV nontunneled HD catheter and a left bracho-cephalic fistula was created. Consequently, the patient was informed that the AVF had failed to mature, and was advised for new AVF creation.
At our institute, there was no blood aspirate from the right IJV non tunneled HD catheter; hence it was removed. Ultrasonography (USG) showed thrombosed right IJV. She was taken up for left femoral tunneled HD catheter insertion.
An Arrow-Clark VectorFlow Antegrade Hemodialysis catheter (15F × 31cm) was placed into the left femoral vein under USG guidance. Following insertion, there was an inability to aspirate blood and the patient complained of inability to flex the hip. Examination showed power of 2/5 at hip joint on flexion. Sensory modalities and reflexes were intact.
The patient was immediately shifted for computed tomography (CT), which showed that the catheter had pierced the posterior aspect of the common iliac vein after initial course within the femoral vein. The catheter further coursed through the retroperitoneum and entered the spinal canal through the left neural foramina of L4 vertebra and coursed cranially to the right neural foramina of L2 vertebra [Figure 1].
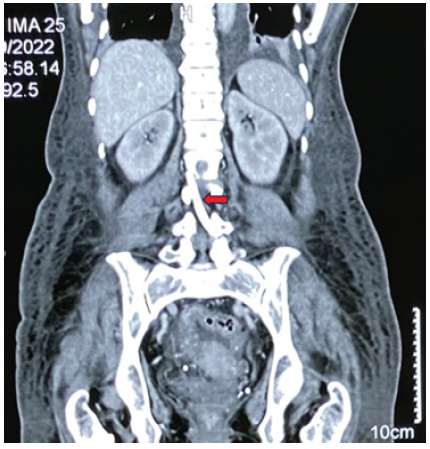
- Computed Tomography (CT) abdomen coronal view. Red arrow marks hyperdense tubular structure (catheter) inside the spinal canal.
The patient was shifted to OT and the catheter was removed by gentle pull followed by local compression on the insertion site. Firm pressure was maintained while simultaneously monitoring blood pressure and pulse rate. Vascular surgeons were present for any exploration required if the patient showed signs of hemodynamic instability.
After 30 min of pressure application, iodinated water soluble low osmolality contrast was injected into the left femoral vein and observed for any extravasation under fluoroscopy. After confirmation of no extravasation of contrast [Figure 2], the patient was shifted back to the ward and 12 hourly hemoglobin monitoring was done in order to detect any delayed bleeding.
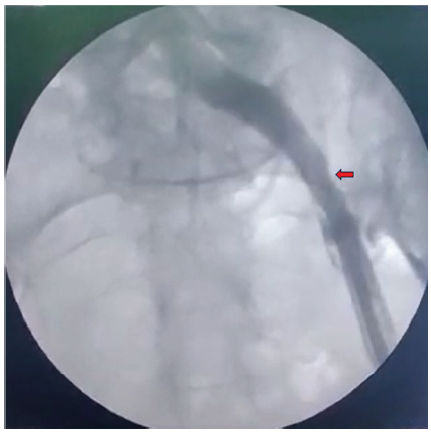
- Fluoroscopic view of the left femoral vein after the catheter had been removed. Red arrow highlights no extravasation of contrast was seen outside the common iliac vein.
There was no drop in hemoglobin over the next 48 hours. Left IJV tunneled HD catheter and tachycardia was placed and right brachiocephalic fistula was constructed.
On follow-up, right brachiocephalic fistula matured after 8 weeks. Left IJV tunneled HD catheter was removed. At 1 year of follow-up, the patient had a left hip power of 4+/5 and was able to walk with support.
Discussion
Despite several drawbacks, more than three-quarters of patients in India are started on dialysis with uncuffed catheter.3 USG-guided tunneled catheter insertion is safe and effective.4
In our patient, the catheter was properly inserted into the femoral vein, but the upstream pathway could not be traced under USG. The complication could have been avoided if the procedure was conducted under fluoroscopy or digital substraction angiography (DSA).
In order to minimise malpositions, some basic precautions must be taken. The operator should have adequate experience in performing USG-guided procedures. The guidewire should only be inserted after the introducer needle has entered the vein. If the introducer needle cannot be visualised, the needle should not be advanced. This prevents injury to surrounding structures. After removing the introducer needle, always sonographically check that the guidewire is within the vein. If resistance is felt anytime, start afresh. If the problem persists, abandon the procedure and attempt later under fluoroscopy or DSA. Force should never be applied to pass the guidewire, dilators, or catheter across a resistance.
If a catheter has been placed and there is inability to aspirate blood, the catheter should not be removed.5 The patient should be shifted for imaging (CT or MRI) to know the exact location of the catheter. Removal may involve a team of interventional radiologists, and vascular and general surgeons.
A well-planned multidisciplinary strategy was undertaken leading to safe removal of the catheter. The lack of internal bleeding after catheter removal was probably due to bleeding into the retroperitoneum that caused a tamponade effect, a possible outcome that we had hoped for before trying the maneuver.
Nephrologists and interventional radiologists should keep in mind the possibility of such an event occurring during tunneled HD catheter insertion through the femoral approach. Adequate precautions should be taken as outlined above to prevent the occurrence of such malpositions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Temporary hemodialysis catheters: Recent advances. Kidney Int. 2014;86:888-95.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Update on insertion and complications of central venous catheters for hemodialysis. Semin Intervent Radiol. 2016;33:31-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Haemodialysis vascular access: Current practices amongst Indian nephrologists. The Journal of Vascular Access. 2018;19:172-6.
- [CrossRef] [PubMed] [Google Scholar]
- Feasibility analysis of ultrasound-guided placement of tunneled hemodialysis catheters. Kidney Int Rep. 2023;8:2001-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Malposition of central venous catheter: Presentation and management. Chin Med J. 2016;129:227-34.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]








