Translate this page into:
Ambulatory Hypertension in Children with Kidney Failure on Maintenance Dialysis
Corresponding author: Priya Pais, Department of Pediatric Nephrology, St John’s Medical College Hospital, Bengaluru, Karnataka, India. E-mail: priyapais@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kamal S, Raj JAM, Pais P. Ambulatory Hypertension in Children with Kidney Failure on Maintenance Dialysis. Indian J Nephrol. 2024;34:503-5. doi: 10.25259/ijn_505_23
Dear Editor,
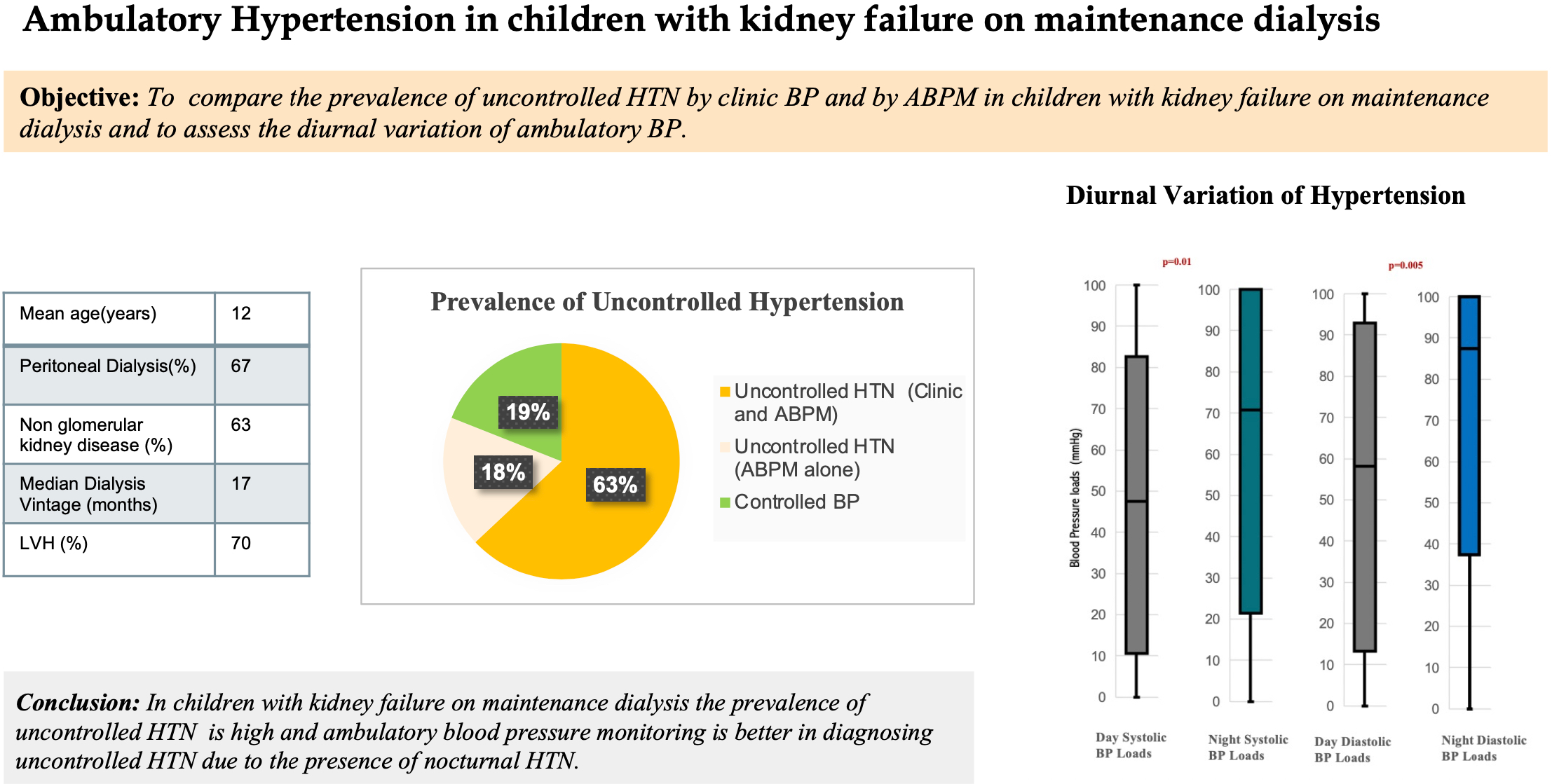
Cardiovascular (CV) disease is the leading cause of death in children with advanced chronic kidney disease (CKD).1 Indian children with CKD have a higher prevalence of CV morbidity compared to the Western pediatric CKD cohort.2 Limited data are available on the prevalence of hypertension (HTN) in children with kidney failure on maintenance dialysis.
Traditionally, blood pressure (BP) in children on dialysis is measured manually in the clinic, which may be inaccurate due to fluctuations in fluid status and diurnal variations.3 Ambulatory BP monitoring (ABPM) has the advantage of detecting diurnal variations in BP over a 24-h period. The objectives of this study were to determine the prevalence of uncontrolled HTN by ABPM versus clinic BP measurement alone in children with kidney failure on maintenance dialysis, to assess the diurnal variation of ambulatory BP and to determine factors associated with ambulatory HTN. For detailed description of methods refer to the Supplementary Material.
Twenty-seven patients (12 ± 2.6 years) consisting of 13 (48%) girls, with 18 (67%) on peritoneal dialysis (PD), having a median dialysis vintage of 17 months (10–35 months) were included. Residual kidney function was present in 16 patients (59%). Concentric left ventricular hypertrophy (LVH) was present in 19 (70%) patients. Twenty-six patients (96%) already had a diagnosis of HTN and were on treatment, with a median of three antihypertensive medications. The patient characteristics are described in Table 1.
| Characteristic | Value |
|---|---|
| Total patients | 27 |
| Girls | 13 (48%) |
| Patients on PD | 18 (67%) |
| Age (years) | 12 (±2.6) |
| Dry wt z-score | −3.2 (±2.3) |
| Ht z-score | −3.18 (±1.9) |
| Non-glomerular native kidney disease | 17 (63%) |
| Dialysis vintage (months) | 17 (10-35) |
| IDWG (wt gain above the dry weight as a percentage of body weight) | 2.5% (±2.16%) |
| Patients with LVH | 19 (70%) |
| HTN by clinic BP alone | 17 (63%) |
| HTN by ABPM | 22 (81%) |
| Isolated nocturnal HTN, n (%) | 4 (18%) |
| Blunted nocturnal dip, n (%) | 24 (89%) |
Data presented as n (%), mean (±SD), or median (IQR). ABPM = ambulatory blood pressure monitoring, DBP = diastolic blood pressure, HTN = hypertension, IDWG = intradialytic weight gain, LVH = left ventricular hypertrophy, PD = peritoneal dialysis, SBP = systolic blood pressure, wt: weight.
Despite the patients being on antihypertensive medication, ABPM identified uncontrolled HTN in 22 (85%) patients and one patient had a newly diagnosed HTN. In contrast, clinic BP monitoring detected uncontrolled HTN in only 17 patients (65%). Therefore, in five patients, HTN was diagnosed only by ABPM (four had masked uncontrolled HTN and one was newly diagnosed). The level of agreement between the clinic BP and ABPM to detect HTN was only moderate (k = 0.5).
All patients with ambulatory HTN were treated with changes in their dialysis prescription or modification of medications.
Mean night-time diastolic BP index was greater than day-time indices (1.19 vs. 0.98, P = 0.001). Night-time BP loads were greater than day-time values (52% vs. 42%, P = 0.01) for systolic BP and (89% vs. 58%, P < 0.001) diastolic BP [Figure 1]. Nocturnal HTN (high night-time BP) was present in 21 patients (78%). Isolated nocturnal HTN was present in 4 (18%) patients. The nocturnal dip was blunted in 24 (89%) patients, with a reversal of dip (higher BP at night-time) found in five of these. The severity of ambulatory HTN did not differ by native kidney disease, dialysis modality, weight gain as a percentage of their dry weight, residual kidney function, or presence of LVH (all P > 0.05).
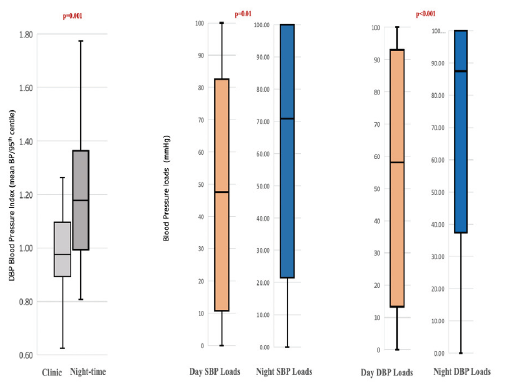
- Diurnal variation of ambulatory blood pressure indices and BP loads. DBP = diastolic blood pressure, SBP = systolic blood pressure.
In our study, we found that 96% of children had clinical diagnoses of HTN and were on salt- and water-restricted diets, regular hemodialysis (HD) or PD, and also antihypertensive medications. Despite these standard clinical measures, uncontrolled HTN persisted in 85% of these patients. The clinical relevance of uncontrolled HTN is likely indicated by the high prevalence of CV morbidity – 70% had concentric LVH (LVH is a known preclinical marker of CV disease in children).
This is the first study in India looking at the ambulatory pattern of HTN in children on dialysis. Prevalence of HTN in our study is higher than that noted in the North American Pediatric Renal Transplant Cooperative Study,4 and the prevalence of uncontrolled HTN is also higher than that of Western pediatric dialysis patients.5 In addition, it is noteworthy that neither of these studies used ABPM.
In our study, almost 20% of patients would have been incorrectly diagnosed with controlled BP if they had been assessed by clinic BP alone. ABPM is better than routine manual BP monitoring at detecting uncontrolled HTN as it reveals nocturnal HTN that is highly prevalent (78%) even in pediatric dialysis patients. Nocturnal HTN occurs in children with secondary HTN, such as those on dialysis, and is an independent risk factor for CV morbidity.6 Thus, we believe that ABPM has an important role in management, even in children who have already been diagnosed with HTN.
Even though native kidney disease, residual kidney function, and weight gain (as a percentage of dry weight) are known to affect ambulatory BP, we could not find statistical associations of these variables with ambulatory HTN in our patients. It is possible that in children on dialysis, HTN is multifactorial, similar to adults, and less affected by factors affecting HTN in earlier stages of CKD.
Due to its retrospective nature, we did not have access to ultrafiltration volumes of the HD or PD sessions preceding the 24-h ABPM period. In an attempt to address the role of salt and water retention as a cause for uncontrolled HTN, we used weight gain (as a percentage of dry weight) as a surrogate marker of fluid overload.
In conclusion, despite the universal use of antihypertensive medication in children on maintenance dialysis, ABPM detected uncontrolled HTN in 85% of patients. ABPM is superior to clinical BP in detecting uncontrolled HTN due to the high prevalence of nocturnal HTN. In this high-risk cohort, studies targeting better nocturnal control of BP are needed to reduce CV risk.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Mortality and cause of death of end-stage renal disease in children: A Dutch cohort study. Kidney Int. 2002;61(2):621-9.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic kidney disease (CKD). An observational study of etiology, severity and burden of comorbidities. Indian J Pediatr. 2017;84(11):822-5.
- [CrossRef] [PubMed] [Google Scholar]
- Hypertension in children with chronic kidney disease: Pathophysiology and management. Pediatr Nephrol. 2008;23(3):363-71.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Hypertension in pediatric patients on long-term dialysis: A report of the North American Pediatric Renal Transplant Cooperative Study (NAPRTCS) Am J Kidney Dis. 2005;45(2):309-15.
- [CrossRef] [PubMed] [Google Scholar]
- Predictors of blood pressure and its control in pediatric patients receiving dialysis. J Pediatr. 2012;160(4):621-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Ambulatory blood pressure monitoring in children and adolescents: A scientific statement from the American Heart Association. Hypertension. 2022;79(7):e114-24.
- [CrossRef] [PubMed] [Google Scholar]






