Translate this page into:
An insight into the sites of noncuffed hemodialysis catheters
Address for correspondence: Dr. H. Mehta, 53A, Heera Panna, Bhulabhai Desai Road, Mumbai - 400 026, Maharashtra, India. E-mail: drhmehta@hotmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Central venous catheters were first described for hemodialysis (HD) vascular access in 1959 by Teschan. Initial approaches required cut down into the saphenous vein to gain access to the inferior vena cava.[1] Later, percutaneous methods of cannulation gained wide acceptance, and reports surfaced in the early 1960s of the more “convenient” double-lumen cannula, which was inserted in the femoral vein. In 1982, Quinton in association with Dr. Sakharam Mahurkar (a nephrologist at County Cook Hospital in Chicago) developed the dual-lumen Mahurkar HD catheter, which remains the standard in acute access for HD and aphaeresis.
Various catheter lengths are available to allow proper positioning of the distal tip. The catheter flow is dependent on the tip position (related to length of catheter) and diameter. The tip of the catheters in neck and groin should be in superior and inferior vena cava, respectively.
The first choice for catheter placement should be the right internal jugular vein (IJV) followed by left IJV. The right internal jugular is seen as the ideal as it has fewer incidence of complications because the dome of the left lung is higher than the right, the thoracic duct empties on the left, and there is a straight course to the superior vena cava on the right. It will reduce the chances of malposition and future central venous obstruction. There is, however, a great variability of the vein caliber and its position in relation to the common carotid artery [Figure 1].[2] Ultrasound guidance is therefore strongly recommended to reduce the 7–10% risk of carotid puncture to virtually zero.[3]
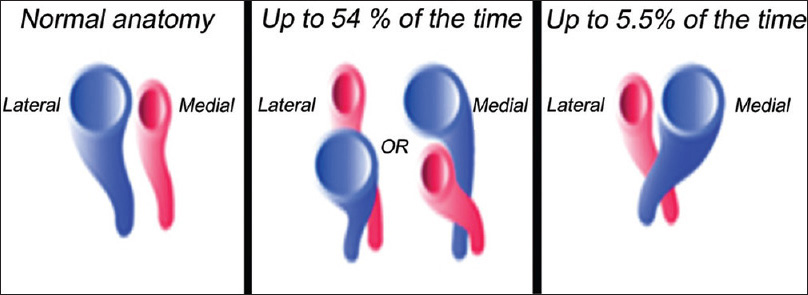
- Anatomical variants of right internal jugular vein
In the right IJV puncture, the three traditional approaches are anterior, posterior and central [Figure 2]. The central approach and posterior approach are most commonly used and are less apt to result in a puncture of the carotid artery. These are used mainly by the anesthesia and critical care personnel. Nephrologists generally use the central approach. This is to ensure better flow due to its position. In this issue, Mathur et al. compare the central vs posterior approach for inserting dialysis catheters.[4] The use of posterior approach for noncuffed HD catheter is a good alternative provided adequate length of catheter is used, and the tip position is proper. The posterior approach moves the point of entry higher up in the neck, thus providing a longer length of vein for cannulation and avoiding the dangers of hemothorax, pneumothorax and carotid puncture, but a larger length catheter will be required. The anterior approach is not used routinely, since the posterior approach in internal jugular venous cannulation is more efficient than (but as safe as) the anterior approach.[5] The posterior approach is also a safe alternate route in obese or short-necked patients.[6] Both anterior and posterior approaches require the patient to be in 30–40° Trendelenburg position, which may be difficult to achieve due to associated orthopnea. Once placed properly, catheter flows may not be a problem. Studies using sonography indicates that needles are less frequently directed toward carotid artery during the anterior and central approach than during the posterior approach. Further, ultrasound-guided prelocation is as effective as ultrasound-guided real-time imaging technique for right IJV cannulation. Both the ultrasound techniques are found to be better than the anatomical landmark technique.[7] The risk of insertion-related complications varies as per the skill of the nephrologist, site of insertion and imaging modality used.[8]
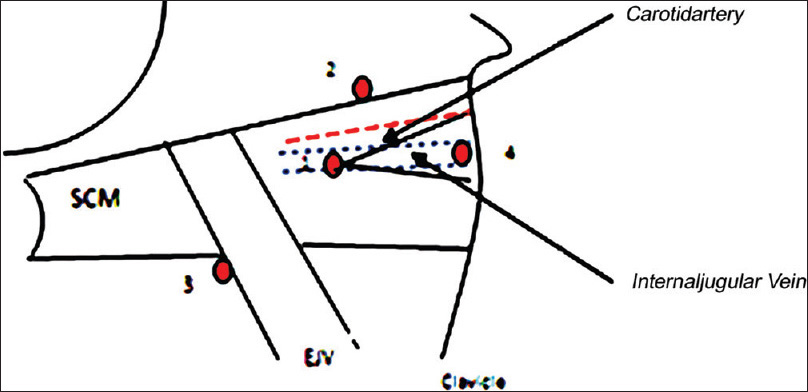
- Sites of right internal jugular vein puncture and its relation with other structures. SCM: Sternocleidomastoid muscle, EJV: External jugular vein (1) central approach, (2) anterior approach, (3) posterior approach, (4) supraclavicular approach
External jugular vein (EJV) can also be used for dialysis catheters. Because of its superficial course, cannulation of EJV is possible in most patients without ultrasound guidance. On both sides, it opens into the subclavian vein almost at a right angle. This occasionally complicates implantation of stiff, large-bore HD catheter, and in the long run will provoke subclavian vein stenosis and thrombosis.[9]
The use of acute noncuffed dialysis catheters in acute situations can be justified, in fact a majority of chronic patients are initiated on dialysis with acute catheters. The use of noncuffed catheters should be restricted to critically ill intensive care unit patients or for “in and out” purpose of those with temporary loss of a permanent access. Use of femoral catheters should be restricted to those unable to lie down, and for not more than 7 days. Acute internal jugular catheters are used for acute situations and for initiation of chronic dialysis patients by centers not using tunneled dialysis catheters. Early fistula placement should be the goal for all chronic kidney disease patients to avoid morbidity associated with acute dialysis catheters and for preservation of central veins. Finally, acute noncuffed dialysis catheters should be restricted to 2 weeks to avoid risks of catheter-related bacteremia and central venous obstruction.
References
- Prophylactic hemodialysis in the treatment of acute renal failure. J Am Soc Nephrol. 1998;9:2384-97.
- [Google Scholar]
- Anatomical variations of internal jugular vein location: Impact on central venous access. Crit Care Med. 1991;19:1516-9.
- [Google Scholar]
- Ultrasound-guided cannulation versus the landmark-guided technique for acute haemodialysis access. Nephrol Dial Transplant. 1997;12:1234-7.
- [Google Scholar]
- A comparative study of central versus posterior approach for internal jugular hemodialysis catheter insertion. Indian J Nephrol. 2015;25:265-8.
- [Google Scholar]
- Internal jugular venous cannulation: What is the best approach? Ann Fr Anesth Reanim. 2012;31:512-6.
- [Google Scholar]
- Comparison of two different approaches for internal jugular vein cannulation in surgical patients. J Postgrad Med. 1998;44:57-62.
- [Google Scholar]
- Internal jugular vein cannulation: A comparison of three techniques. J Anaesthesiol Clin Pharmacol. 2013;29:367-71.
- [Google Scholar]
- Central venous catheters: Many questions, few answers. Nephrol Dial Transplant. 2002;17:1368-73.
- [Google Scholar]






