Translate this page into:
Dialysis Practices Across India - A Nationwide Study
Corresponding author: Abhijit Konnur, Department of Nephrology, Muljibhai Patel Urological Hospital, Nadiad, Gujarat, India. E-mail: abhikonnur@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Konnur AM, Shete NB, Sahay M, Karishetti M, Dhaygude SV, Anandh U, et al. Dialysis Practices Across India - A Nationwide Study. Indian J Nephrol. doi: 10.25259/IJN_410_2024
Abstract
Background
The practise of hemodialysis (HD) is highly variable in terms of geographical distribution, medical enterprises, human resources allocation, financial support, and type of population. This study aims to examine the dialysis practices across participating centers in an incident end-stage kidney disease study in India.
Materials and Methods
Thirty dialysis centers across West, Central, and Southern India were enrolled in April 2019 as part of a point prevalence cross-sectional multicentric descriptive study to examine dialysis practice patterns. Only centers providing more than 500 dialyses per month and a minimum of 10 machines were included. Data were collected using electronic forms.
Results
The distribution of dialysis centers as per ownership was divided into government, private, and public–private partnership (PPP) models, with 4 (13.33%), 7 (23.33%), and 19 (63.33%) each, respectively. The majority (36.67%) of the dialysis centers housed 11–20 dialysis stations. Two (6.67%) of the centers were of large volume, catering > 40 dialysis stations. Around 90% of the dialyzers were reused 4–6 times before discarding. Most centers (50%) performed less than 1000 dialysis per month. All centers had water treatment plants with deionizer and used carbon filters and reverse osmosis technology. Around 93% of the centers used UV light for disinfection. 56.6% of the plants used nonstandardized analysis for chemical assessment of the quality of treated water, while 66.67% utilized culture and sensitivity for microbiological assessment of treated water quality. Patient segregation policy was followed in 93% of the centers, and all centers had qualified nephrologist coverage.
Conclusion
Indian hemodialysis centers are mostly stand-alone and cater to a low to medium volume of end-stage renal disease patients. There has been a shift from privately run dialysis units in the past to the PPP model of dialysis delivery. Most dialysis centers have a quality control mechanism in place.
Keywords
Hemodialysis
Multicentric
Dialyzer
Water quality
Introduction
Hemodialysis (HD) was introduced in India in the year 1961.1 Despite being the most common mode of end-stage kidney disease (ESKD) care, there has been a paucity of data on the outcomes of maintenance hemodialysis (MHD). As of 2018, there were around 13,000 dialysis stations in India.2 The National Dialysis Program, introduced in 2016 to cater to dialysis patients from poor households, has added another 8000 dialysis stations in government hospitals or through the private–public partnership (PPP) model.3 However, the dialysis demand is not fully met, as the projected number of patients in India with ESKD is close to 1.75 million.4 Most HDs in India are in the nongovernmental sector, where the expenses are met through either insurance (private or government-sponsored) or out-of-pocket (OOP). Employer-sponsored programs often give higher reimbursement rates; however, they are accessible only to a few. The average cost of an HD session varies from INR 600–5000 (USD 8–62).5 Despite the subsidized care and widespread availability of dialysis, a few months on dialysis can pose a substantial financial burden. Single-center studies have estimated that 40–93% of the patients on HD face a catastrophic healthcare burden.6
There is a broad range of practice patterns related to HD regarding prescriptions, frequency, duration, access, and medications. In 2009, The Indian Society of Nephrology published guidelines for providing MHD, which the Ministry of Health and Family Welfare, Government of India, later declared as its guidelines for MHD.7 However, there is no evidence that the guidelines are followed, and there is scarce evidence of the outcomes of patients on MHD. Even more glaring is the information deficit related to HD center infrastructure, delivery mechanisms and efficiency and their relation to the mortality and morbidity.8-12 Hemodialysis center ergonomics, availability of healthcare experts such as physiotherapists, occupational therapists, dieticians, trained dialysis technicians, and nurses, and their relation to survival and quality of life (QOL) of patients is unknown. This study looks at one aspect of dialysis delivery in India, the types of centers and their practice patterns.
Materials and Methods
The “Shree Narayandasji Santram Maharaj improving hemodialysis outcomes initiative” is a multicenter, observational study to assess patient survival and QOL of incident MHD patients. This manuscript reports the results of a point prevalence cross-sectional descriptive study. Data were collected from 30 dialysis centers across West, Central, and Southern India. encompassing dialysis centers in governmental, private, and nongovernmental nonprofit–based organizations and PPP-based centers. A steering committee, comprising the principal investigators from all centers, developed the study protocol. The protocol was harmonized to capture data in a standardized manner to facilitate comparisons across reputed international dialysis registries. Individual Institutional Ethics Committee approvals were obtained from all collaborating centers and the Nodal Center at Muljibhai Patel Urological Hospital, Nadiad.
The data were captured in a proforma, which included center demographics, dialysis-associated information on machines, manpower, dialyzer and tubing information, water treatment protocols, infection control practices, and education facilities.
Study population
At the onset of the study, only centers with more than 500 dialyses per month and a minimum of 10 machines were included. Many large centers across India were approached to participate in the study. As the enrollment progressed, some centers with less than 500 dialysis sessions per month and less than 10 dialysis machines were also included as the recruitment number for centers was low. The enrollment started on April 1, 2019, and the expected duration is until June 2027. The data was collected using electronic forms online (www.snsmds.org).
The data were exported to Microsoft Excel, cleaned, and descriptive statistics were used to present the data.
Results
A total of 30 centers from Gujarat, Maharashtra, Karnataka, Kerala, Puducherry, Telangana, and Tamil Nadu participated [Figure 1]. The distribution of dialysis centers was divided into government, private, and PPP models, with 4 (13.33%), 7 (23.33%), and 19 (63.33%), respectively. The majority (36.67%) of the centers housed 11–20 dialysis stations. Two (6.67%) large-volume centers catered > 40 dialysis stations [Table 1]. Around 90% of dialyzers were reused 4–6 times (56.67%). Most of the centers (50%) performed less than 1000 dialyses per month. Of the 1039 incident ESKD patients studied at these centers, 556 (53.66%) underwent two dialyses per week, and 480 (46.33%) underwent three dialyses per week [Table 1].
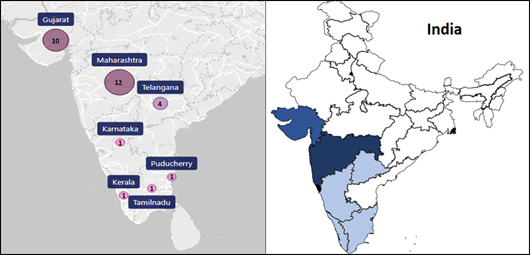
- Participating center distribution in India and geographical representation of the study population.
| Total centers involved in study = 30 | No. of center (%) |
|---|---|
| No. of dialysis stations | |
| <=20 | 20 (66.67) |
| 21–30 | 4 (13.33) |
| 31–40 | 3 (10) |
| 41–50 | 2 (6.67) |
| Dialyzers used | |
| Fresenius | 17 (56.67) |
| Nipro | 2 (6.67) |
| Fresenius + Nipro | 2 (6.67) |
| Others | 9 (30) |
| Type of tubing used | |
| Nipro | 15 (50) |
| Fresenius | 9 (30) |
| Others | 6 (20) |
| Dialyzer re-used | |
| Yes | 27 (90) |
| No | 3 (10) |
| Times reused | |
| 1–3 | 2 (6.67) |
| 4–6 | 17 (56.67) |
| 7–9 | 4 (13.33) |
| 10–12 | 4 (13.33) |
| Dialysis performed (Avg. PM) | |
| <1000 | 17 (56.67) |
| 1000–2000 | 10 (33.33) |
| 2000–3000 | 2 (6.67) |
| >3000 | 1 (3.33) |
PM: Per month
These centers had 1–5 dialysis delivery–related personnel, of which 73.3% were female nurses and 60% were male technicians. There were no female nursing staff in 3 centers (10%), and 16 centers had no male nursing staff (53.33%). Six centers had no female technician staff (20%) [Table 2] [Supplementary File].
| Workforce | Nurse | Technicians | ||
|---|---|---|---|---|
| Male | Female | Male | Female | |
| Single-gender workforce | 17 (56.67) | 4 (13.33) | - | 6 (20) |
| 1–5 | 11 (36.67) | 22 (73.33) | 18 (60) | 17 (56.67) |
| 6–10 | - | - | 9 (30) | 5 (16.67) |
| 11–15 | - | - | 2 (6.67) | 1 (3.33) |
| 16–20 | 1 (3.33) | 1 (3.33) | 1 (3.33) | 1 (3.33) |
| >20 | 1 (3.33) | 1 (3.33) | - | - |
Note that each cell in the above table gives the no. of centers (%).
All centers had water treatment plants with deionizer usage. Twenty-nine centers used carbon filters, of which 80% used a single filter and 20% used two filters in a series. Reverse osmosis (RO) technology was used in all 30 centers; 83.3% used a single RO membrane, while 16.6% used two membranes in a series. UV light was used for disinfection by 93%. 56.6% of the plants used nonstandardized analysis for chemical assessment of treated water quality, while 66.67% utilized culture and sensitivity for microbiological assessment of treated water quality. Endotoxin assessment using the LAL test was utilized in 50% of centers. Most centers conducted water quality assessments every quarter or less [Table 3].
| No. of centers (%) | |||
|---|---|---|---|
| Physical assessment for water quality | |||
| Water treatment system | 30 (100) | ||
| Water deionizer usage | 30 (100) | ||
| Carbon filter (single filter/two filters in series) | 24/6 (80/20) | ||
| Reverse osmosis (single RO/two RO in series) | 25/5 (83.33/16.67) | ||
| Ultraviolet disinfection (Yes/No) | 28/2 (93.3/2.67) | ||
| Chemical assessment for water quality | |||
| AAMI criteria | 3 (10) | ||
| Atomic mass spectrometry | 7 (23.33) | ||
| Other chemical analysis methods# | 17 (56.67) | ||
| None | 3 (10) | ||
| Microbiological assessment for water quality | |||
| Culture and sensitivity | 20 (66.67) | ||
| Other tests* | 7 (23.33) | ||
| None | 3 (10) | ||
| Pyrogen method for water quality | |||
| LAL test | 15 (50) | ||
| Others** | 12(40) | ||
| None | 3 (10) | ||
| Method for water quality check versus how often used? | Chemical | Microbiological | Pyrogen |
| (0–4) months | 17 (56.67) | 26 (86.67) | 21 (70) |
| (4–8) months | 9 (30) | 1 (3.33) | 6 (20) |
| (8–12) months | 1 (3.33) | - | - |
| Patient segregation policy | |||
| Patient segregated (Yes/No) | 28/2 (93.3/2.67) | ||
#Online RO, Local chemical analysis, magnetic particle test, sieve analysis, ultrasound test, pH test, TDS test *Gramocid, Tap water culture, membrane filtration technique, Pour plate and ytek **Loop method, clot reagent method, Microtech, RO: Reverse osmosis, AAMI: The Association for the Advancement of Medical Instrumentation, LAL: Limulus amebocyte lysate assay
Patient segregation policy was followed in 93% of the centers to prevent cross-contamination due to viruses.
All centers had qualified nephrologist coverage. Three centers had full-time nephrologists, while 27 had daily nephrologist visits. Technician Training Course was available in 14 centers.
Discussion
A large proportion of dialysis centers had moderate volume (11–20 dialysis stations) and delivered small to medium volumes of dialysis (less than 1000 per month). Large-volume centers were very few.
All centers were covered by nephrologists. These findings were similar to the study by Agarwal et al., which noted that there were more than 820 nephrologists distributed in North (35.5 %), South (30%), West (23%), East (9%), and Central India (2.5%).13 Their study highlighted that more than 710 HD units had more than 2500 dialysis stations, with the average being 3 (range 2–24) stations per unit. On average, two dialyses were performed per station daily.12 In our study, 33.3% of the dialysis centers performed 1000–2000 dialysis per month. Regarding accessibility to HD facilities in different states, 17 (56.67%) were low-volume centers, performing less than 1000 dialysis per month.
There has been a paradigm shift in the dialysis scenario in India. During 1990–2010, nearly 85% of the centers were privately run and performed both transplant-oriented dialyses and MHD.2 At that time, it was espoused that as opposed to the private sector, the government sector could not afford to provide MHD, and thus only operates renal transplant-oriented HD facilities. From this study, it is clear that there is a majority of stand-alone dialysis centers.
The number of HD beds in India was estimated at 12,881 in 2018.2 The Indian government announced a National Dialysis Program in 2016, which envisaged setting up an eight-station dialysis facility in all 688 districts of the country to provide HD to poor patients. India being predominantly rurally populated, almost 60% of patients on dialysis had to travel more than 50 km to access HD, and nearly a quarter stayed 100 km away from the nearest facility.2 The travel costs and loss of wages add to the dialysis burden. The long commute and the accompanying revenue losses were the major reasons for dropout, even when dialysis was provided at subsidized rates. With the advent of government-assisted dialysis programs in district and taluk hospitals, many patients have an accessible dialysis station at a short distance; often in many centers, the travel expenses are reimbursed as well.
Disproportionately large volumes of centers have Fresenius dialysis machines (56.67%). Conversely, a disproportionately large volume of centers (50%) use Nipro dialyzer tubings. These point to the overt dependency of dialysis centers on the two major companies predominantly.
Although 90% of dialyzers are reused 4–6 times before discarding them, in our resource-limited setting, reusing dialyzers may curtail costs and burden the environment.
All centers had water treatment plants with advanced sterilization technology and surveillance protocols for physical, chemical, and microbiological quality. The frequency of surveillance was also satisfactory and as per the recommendations.
There were some limitations to this study. Centers were limited to West and South India, and hence may not reflect dialysis patterns across the whole country. The point prevalence study design does not shed light on changes in dialysis patterns in centers and their effects on patient survival or QOL. The segregation policy, sterilization procedures, dialysis dose and duration of sessions, dialyzer reuse using machine and manual methods, and reuse protocols have not been studied in detail.
Indian HD centers are mostly stand-alone and cater to low to medium volume of ESRD patients. There is a shift from private-run dialysis units in the past to PPP model of dialysis delivery. Dialysis machines and tubings are sourced from two major companies with dialyzer reuse being common. Most dialysis centers have a quality control test in place.
Acknowledgments
We express our gratitude to Dr. M. M. Rajapurkar (MD) for his technical and general support and for arranging financial help, Devangbhai Patel and Santram Mandir for their patronizing help in carrying out the study, and Ms Mansi and Mr Kalpesh Desai for their technical support with online program design.
Financial support and sponsorship
Muljibhai Patel Society for Research in Nephro-Urology for financial support. The funding agency had no role in the actual conduct of the study.
Conflicts of interest
There are no conflicts of interest.
References
- Differences in the care of ESRD patients worldwide: Required resources and future outlook. Kidney Int Suppl. 1995;50:S7-13.
- [Google Scholar]
- Cost of hemodialysis in a public sector tertiary hospital of India. Clin Kidney J. 2018;11:726-33.
- [Google Scholar]
- Paying for hemodialysis in Kerala, India: A description of household financial hardship in the context of medical subsidy. Kidney Int Rep. 2018;4:390-8.
- [Google Scholar]
- Indian hemodialysis guidelines. http://www.clinicalestablishments.gov.in/WriteReadData/8451.pdf
- National and international kidney failure registries: Characteristics, commonalities, and contrasts. Kidney Int. 2022;101:23-35.
- [Google Scholar]
- What do we know about chronic kidney disease in India: First report of the Indian CKD registry. BMC Nephrol. 2012;13:10.
- [Google Scholar]
- The indian chronic kidney disease (ICKD) study: baseline characteristics. Clin Kidney J. 2021;15:60-9. doi: 10.1093/ckj/sfab149. PMID: 35035937; PMCID: PMC8757418
- [Google Scholar]
- Utilization, costs, and outcomes for patients receiving publicly funded hemodialysis in India. Kidney Int. 2018;94:440-5.
- [Google Scholar]
- Haemodialysis for end-stage renal disease in Southern India--a perspective from a tertiary referral care centre. Nephrol Dial Transplant. 1998;13:2494-500.
- [Google Scholar]
- Chronic kidney disease in India: Challenges and solutions. Nephron Clin Pract. 2009;111:c197-203. discussion c203
- [Google Scholar]








