Translate this page into:
Evolution of Proliferative Glomerulonephritis with Monoclonal Immunoglobulin Deposits Over a Decade
Corresponding author: Dipankar Bhowmik, Department of Nephrology, All India Institute of Medical Sciences, Ansari Nagar, New Delhi - 110 029, India. E-mail: dmbhowmik@aiims.edu
-
Received: ,
Accepted: ,
How to cite this article: Bhowmik D, Singh G, Mandal S, Dhawan R, Balakrishnan M, Duggal R. Evolution of Proliferative Glomerulonephritis with Monoclonal Immunoglobulin Deposits Over a Decade. Indian J Nephrol. 2024;34:514-5. doi: 10.4103/ijn.ijn_357_23
Abstract
Infections remain an important cause of morbidity in kidney transplant recipients, particularly in the early post-transplant period. This window coincides with an increased risk of acute rejections. Prompt identification of the cause of graft dysfunction is paramount to ensure good outcomes. This case report presents a 32-year-old male undergoing his second living-related kidney transplantation, complicated by herpes simplex virus-2 (HSV-2) nephritis. Despite favorable initial graft function, he developed odynophagia post-operatively, leading to the diagnosis of HSV-related esophageal ulcers. Subsequent acute graft dysfunction prompted biopsy, revealing HSV-2 related acute tubular injury. Prompt initiation of intravenous acyclovir resulted in graft recovery. This case underscores the importance of considering uncommon viral etiologies in post-transplant complications and highlights the role of timely diagnosis and treatment in preserving graft function.
Keywords
Herpes simplex virus-2 Nephritis
HSV nephritis
post-transplant viral infections
graft dysfunction
kidney transplantation
acute rejection
Introduction
Monoclonal gammopathy of renal significance (MGRS) is diagnosed by the presence of monoclonal deposits by immunofluorescence on renal biopsy in a patient who would otherwise be diagnosed as monoclonal gammopathy of unknown significance.1 The spectrum of MGRS is wide and includes proliferative glomerulonephritis with monoclonal deposits (PGNMID).2 The light microscopic feature of PGNMID is that of membranoproliferative glomerulonephritis (MPGN) or proliferative glomerulonephritis. The frequently deposited immunoglobulin is Immunoglobulin3 with kappa light chain restriction.3 The natural history of PGNMID is not well characterized. We report a patient with PGNMID with three renal biopsies over a 10-year period.
Case Report
A 47-year-old female had a history of hypertension and edema in 2013. She showed elsewhere and was detected to have nephrotic syndrome with serum creatinine 1.5 mg%. Kidney biopsy showed immune complex MPGN. Immunofluorescence study (IF) then did not show any monoclonal restriction, with both kappa and lambda staining being of equal intensity. She was put on conservative treatment (without immunosuppression) and remained stable for the next eight years. Two years back, she developed anasarca and worsening renal functions and presented to the renal clinic in AIIMS. Her proteinuria was 5.1 g/day, and serum creatinine was 2.7 mg%. Repeat renal biopsy showed a similar pattern of renal involvement with a questionable preponderance of kappa deposition on IF. Initially, she was managed conservatively with diuretics and ARBs; however, with increasing proteinuria of 17 g/day, she was given a trial of steroids from May 2022. However, around four months later, she developed rapidly worsening renal function with anasarca and nephrotic range proteinuria. The third renal biopsy showed MPGN [Figure 1] with definite kappa restriction on immunofluorescence [Figure 2] of the Immunoglobulin3 subtype along with C3 and C1q 3+ positivity. Bone marrow biopsy did not show any increase in plasma cell population. Whole-body PET-CT did not show any metabolically active lesion. The serum creatinine increased steadily to 7.5 mg/dL. She was treated with three 500-mg doses of injection methylprednisolone and four 500-mg doses of injection cyclophosphamide. Oral prednisolone was started after the injection of methylprednisolone pulses. The renal functions gradually improved, but nephrotic range proteinuria persisted. She was then started on a cyclophosphamide, bortezomib, and dexamethasone (CyBorD) regimen. The edema disappeared, proteinuria subsided gradually (currently UPCR-2.5), serum albumin increased to 3.8 g/dL, and creatinine is currently stable at 2.3 mg/dL. A total of six cycles of the CyBorD regimen is planned to be administered.

- Membranoproliferative glomerulonephritis with extracapillary crescent formation. Tubulo-interstitial chronicity is minimal (PAS stain × 400).
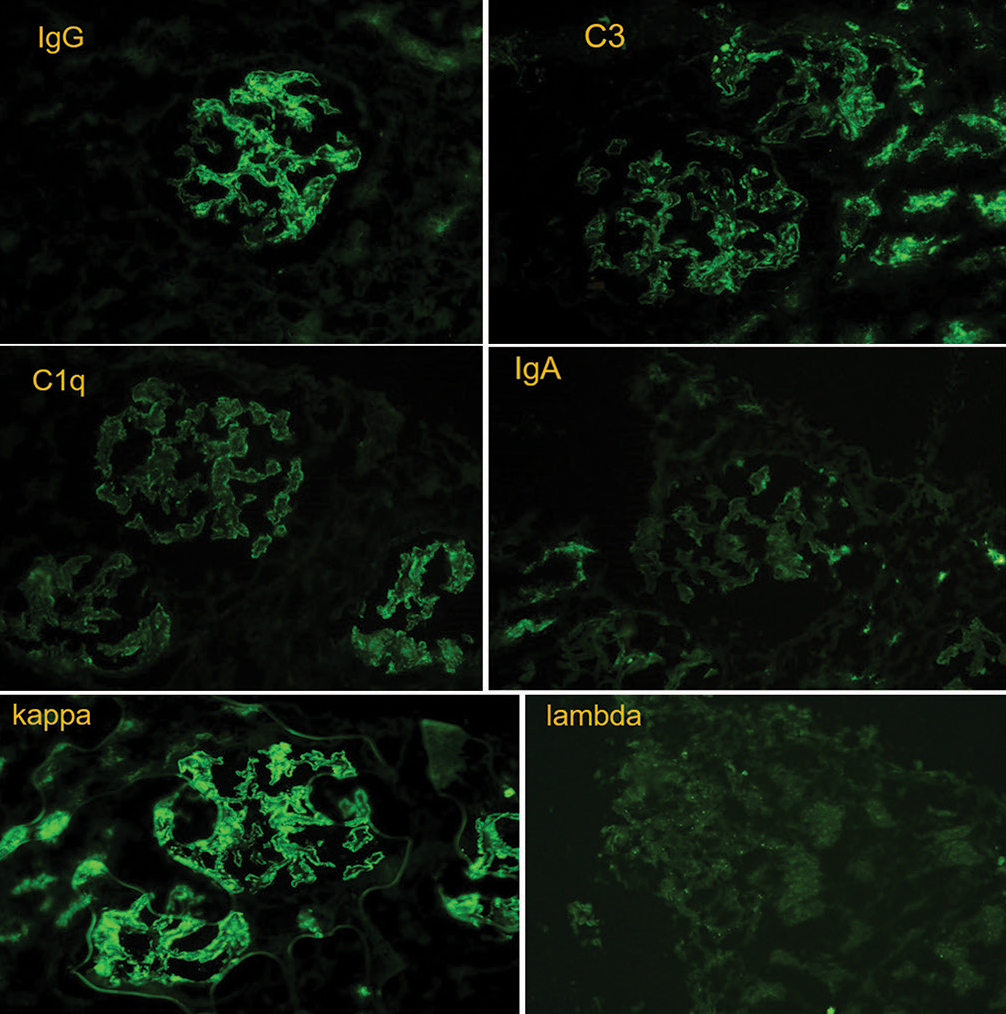
- Immunofluorescence microscopy showing glomerular deposits stained with anti-Immunoglobulin and anti-kappa (light chain) antibodies. Anti-lamba staining is notably absent (x400).
Discussion
Unique features of this case include three kidney biopsies over a period of 10 years and crescentic transformation of MPGN, which is quite rare.4,5 In our patient, the initial biopsy showed idiopathic MPGN, and the course was relatively benign for the first eight years. Thereafter, proteinuria increased, and in the second biopsy, there was a slightly higher kappa preponderance. Subsequently, she suddenly developed features of rapidly progressive glomerulonephritis with nephrotic syndrome. The third kidney biopsy showed classical PGNMID with crescentic transformation. Detailed investigations did not reveal any systemic clone, and she responded reasonably well to CyBorD therapy. One possibility is that she initially had idiopathic MPGN followed by the development of PGNMID. However, it may be more likely that it was the same disease process from the beginning, which evolved over 10 years. A similar case with a 46-year follow-up was recently reported from the USA.6 However, other detailed investigations were not done. Ours is the first such case with a long follow-up from India. PGNMID cases should be treated with clone-directed therapy. Often no clone is found, as in our patient. In such a scenario, standard anti-myeloma therapy is given with a variable response. Fortunately, our patient did well. These two cases are a step forward toward the elucidation of the natural history and appropriate treatment of PGNMID.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
References
- Kidney Transplantation and monoclonal gammopathy of undetermined significance. Transplant Direct. 2021;7:e723.
- [CrossRef] [PubMed] [Google Scholar]
- A fresh perspective on monoclonal gammopathies of renal significance. Kidney Int Rep. 2021;6:2059-65.
- [CrossRef] [PubMed] [Google Scholar]
- Proliferative glomerulonephritis with monoclonal immunoglobulin deposits: A nephrologist perspective. Nephrol Dial Transplant. 2021;36:208-15.
- [CrossRef] [PubMed] [Google Scholar]
- Crescentic glomerulonephritis developing in the course of idiopathic membranoproliferative glomerulonephritis. Saudi J Kidney Dis Transpl. 2023;24:333-7.
- [CrossRef] [PubMed] [Google Scholar]
- Filgastrim-induced crescentic transformation of recurrent Immunoglobulin2λ GN. J Am Soc Nephrol. 2016;27:1911-5.
- [CrossRef] [PubMed] [Google Scholar]
- Proliferative glomerulonephritis with monocolonal Immunoglobulin deposits: A unique case with a clinical course of over 46 year. BMC Nephrol. 2023;24:109.
- [CrossRef] [PubMed] [Google Scholar]







