Translate this page into:
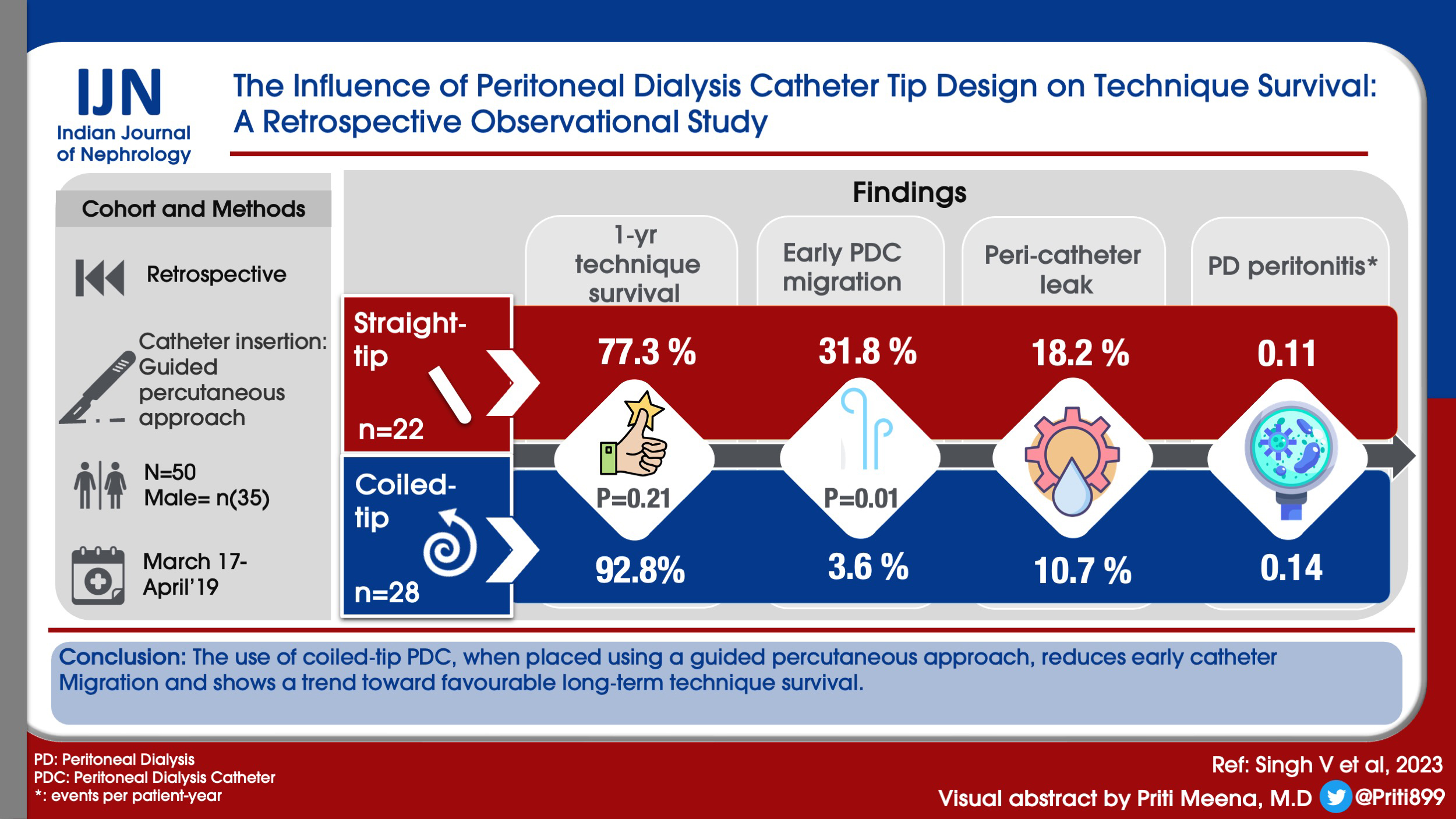
The Influence of Peritoneal Dialysis Catheter Tip Design on Technique Survival: A Retrospective Observational Study
Address for correspondence: Dr. Vishal Singh, Department of Medicine, Division of Nephrology, 7 Air Force Hospital, Kanpur Cantt, Uttar Pradesh – 208004, India. E-mail: vishal23415@gmail.com
-
Received: ,
Accepted: ,
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
The clinical practice guidelines for peritoneal access state that no particular peritoneal dialysis catheter (PDC) type has been proven superior to another. We present our experience with the use of different PDC tip designs.
Method:
The study is a retrospective, real-world, observational, outcome analysis correlating the PDC tip design (straight vs. coiled-tip) and technique survival. The primary outcome was technique survival, and the secondary outcome included catheter migration and infectious complications.
Result:
A total of 50 PDC (28 coiled-tip and 22 straight-tip) were implanted between March 2017 and April 2019 by using a guided percutaneous approach. The 1-month and 1-year technique survival in the coiled-tip PDC was 96.4% and 92.8%, respectively. Of the two coiled-tip catheters lost, one was a consequence of the patient having undergone live related kidney transplantation. The corresponding 1-month and 1-year technique survival with straight-tip PDC was 86.4% and 77.3%, respectively. When compared to straight-tip PDC, the use of coiled-tip PDC was associated with fewer early migration (3.6% vs. 31.8%; odds ratio (OR): 12.6; 95% confidence interval (CI): 1.41–112.39; P = 0.02) and a trend toward favorable 1-year technique survival (P = 0.07; numbers needed to treat = 11). Therapy-related complications noted in the study included peri-catheter leak and PD peritonitis. The PD peritonitis rate in the coiled-tip and straight-tip group was 0.14 and 0.11 events per patient year, respectively.
Conclusion:
The use of coiled-tip PDC, when placed using a guided percutaneous approach, reduces early catheter migration and shows a trend toward favorable long-term technique survival.
Keywords
Coiled-tip PD catheter
straight-tip PD catheter
technique survival
urgent start PD
Introduction
The rising prevalence of chronic kidney disease (CKD) in the general population represents a major health care concern.[1] Many of these patients with CKD progress to end-stage renal disease (ESRD) and require renal replacement therapy. Kidney transplantation, the therapeutic gold standard, is limited by the supply-demand mismatch, cost, and the availability of technical expertise. Hemodialysis (HD) and peritoneal dialysis (PD) are thus life-sustaining. Although HD remains the preferred dialysis modality worldwide, it requires a dedicated setup, trained manpower, uninterrupted electricity, and a vascular access capable of providing rapid extracorporeal blood flow. Many of these are unavailable in a resource-poor environment. PD by virtue of its simplicity offers an attractive alternative.[2] It is simple to perform, preserves the residual renal function (RRF), and does not require significant technical support or electricity.
The key to the successful delivery of PD is a reliable, well-functioning permanent PD catheter (PDC). Catheter failure represents a prominent etiology for dropout from PD and conversion to HD.[3,4] In an endeavor to reduce PDC-related complications, many modifications in the catheter design have been proposed and studied. One such modification was the alteration in the terminal intraperitoneal part of the PDC from a straight to a coiled-tip configuration. It was assumed that coiled-tip PDC by virtue of the bulk of the tubing would ensure better separation between the parietal and the visceral layer of the peritoneum, thus improving the fluid flow, reducing the dialysate infusion pain, and protecting the PDC tip from migration. However, the results have been conflicting and form the basis of current recommendations, which do not favor one catheter design over another.[5] These recommendations are based on studies with many limitations. A vast majority of them are over half a decade old and included multiple simultaneous interventions with respect to the catheter configuration and surgical methodology. Moreover, the technique involved was predominantly surgical, and the data pertains to patients of European or Chinese ancestry. Over the years, there has been a paradigm shift, with PDC increasingly being placed by interventional nephrologists by using a percutaneous approach under fluoroscopic guidance. The existing conclusions derived from surgical techniques cannot be extrapolated to other catheter implantation methodologies. Thus, there is a need to revisit the relationship between the PDC tip design with technique survival following guided percutaneous PDC placement in Indian patients.
Material and Method
Study design: This is a retrospective, real-world observational study. The aim of the study was to study the relationship between PDC tip configuration with technique survival and to determine whether there is a clinical advantage for one over another.
Subject and method: The study was initiated at a government-run tertiary care center in southern India. It was subsequently continued at an affiliated hospital in northern India. Approval for collation and analysis of data was obtained from the institutional ethics committee of both hospitals. The data for all PDC placed percutaneously by an interventional nephrologist between March 2017 and April 2019 were retrieved from the institutional PD record book and analyzed. The last outpatient visit was taken as the duration of follow-up.
Inclusion criteria: All patients with CKD requiring RRT who choose PD as a dialysis modality.
Exclusion criteria:
(a) Major abdominal surgery in the past or a history suggestive of intra-abdominal adhesion.
(b) Persistent coagulopathy with an international normalized ratio of more than 1.5 despite the administration of fresh frozen plasma.
(c) Morbid obesity (body mass index, weight in kilograms divided by the square of height expressed in meters greater than 35)
The choice of the catheter: The choice between straight and coiled-tip PDC, both having medical-grade silicon rubber, was based on the availability. The straight-tip PDC used included a 42-cm, 2-cuff Tenckhoff catheter (Covidien LLC, 15 Hampshire Street, Mansfield, MA 02048 USA). The curled-tip PDC used was a 63-cm coiled catheter with a double cuff (medCOMP, 1499 Delp Drive, Harleysville, PA 19438).
Technique used: All PDCs were placed in an interventional radiology suite under guidance [Figure 1]. Complete blood count, blood grouping, coagulation parameters, and informed written consent were obtained before the procedure. The insertion site and the exit site were planned taking into consideration the beltline, skin creases, obesity, and presence of scars if any. A single preoperative dose of intravenous prophylactic antibiotics was given prior to the surgery. The technique used was percutaneous needle-guidewire by using the modified Seldinger technique. The course of guidewire, introducer sheath, and the catheter were monitored in real time using fluoroscopy. The performance of the PDC and its position were assessed clinically and fluoroscopically, respectively.
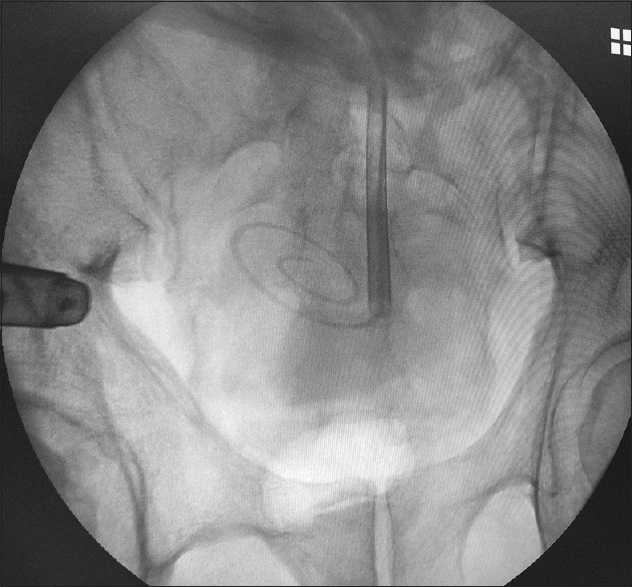
- Fluoroscopic image showing appropriate delivery and placement of the coiled-tip peritoneal dialysis catheter
PD initiation and follow-up: The protocol used was chronic urgent-start recumbent PD by using a low dwell volume (20 mL/kg/exchange) with an incremental approach. The short break-in period was a clinical necessity to circumvent the need for temporary HD, as the majority of the patients presented with either advanced symptomatic azotemia or converted from HD to PD due to a lack of vascular access. In the event of a peri-catheter leak, PD was stopped for 48 h and the patient was reassessed. All the patients underwent in-center training from day 5 onwards and were subsequently followed up at monthly intervals.
Outcome: The primary outcome studied was 1-month and 1-year technique survival. The secondary outcome included catheter migration and catheter-related infectious complications. The various outcome variables were predefined as per the center policy.
(a)Catheter tip migration: The PDC tip was deemed to have migrated if the tip was visualized outside the pelvic brim on an X-ray scan. It was further subclassified as early (<8 weeks) or late (>8 weeks). The migration was deemed irreversible if it failed to reposition despite intervention including ambulation, purgative enema, and fluoroscopy-guided manipulation using a stiff guidewire.
(b)Drainage dysfunction: Inability to drain 80% of instilled PD fluid within 45 min.
(c)Peri-catheter leak: The leakage of PD fluid either externally from around the PDC or internally into the subcutaneous tissue.
(d)PD peritonitis: The presence of two of the following: (i) symptoms and signs of peritoneal inflammation; (ii) cloudy peritoneal fluid with an elevated peritoneal fluid cell count (>100/mL); (iii) demonstration of bacteria in the peritoneal effluent by Gram stain or culture.
(e)Exit site infection: The presence of purulent discharge with local peri-catheter erythema and or tenderness.
(f)Tunnel infection: The presence of erythema, tenderness, or swelling over the PDC subcutaneous tunnel pathway.
(g)Technique survival: The ability to continue performing PD with a good inflow and outflow while achieving the desired dialysis dose. Technique failure was defined as a change in modality from PD to hemodialysis due to any cause, including mechanical and infectious complications.
Statistical analysis: Data were extracted and tabulated using a Microsoft Excel spreadsheet. The categorical variables were expressed as frequency and percentage, and a comparison of proportion was performed using two-tailed Fisher’s exact test. The distribution of quantitative variables was assessed for normality and expressed as mean ± standard deviation. The mean between the two independent groups was compared using paired t test. Statistical analyses were performed using GraphPad Prism 5.0 (GraphPad Software, Inc., San Diego, CA). P < 0.05 was accepted as statistically significant.
Result
The study population comprised 50 consecutive patients, including 35 men and 15 women. Based on the PDC tip design, two groups were identified: coiled-tip (n = 28) and straight-tip (n = 22) [Table 1]. A vast majority had comorbidities, including hypertension and type 2 diabetes mellitus. Diabetic kidney disease was the most common etiology for ESRD. The nutritional status of the two groups assessed using body mass index, mid-arm circumference, and serum albumin were similar in the two groups.
| Coiled-tip PDC (n=28) | Straight-tip PDC (n=22) | P | |
|---|---|---|---|
| Age in years (mean, SD) | 57.4±8.5 | 55.5±11.2 | 0.49 |
| Male Sex | 21 (75%) | 14 (63.6%) | |
| Formal education (n, %) | |||
| Nil | 5 (17.9%) | 3 (13.6%) | 1.00 |
| School | 9 (32.1%) | 9 (40.9%) | 0.56 |
| College | 14 (50%) | 10 (45.5%) | 0.78 |
| Gainfully employed | 6 (21.4%) | 4 (18.2%) | 1.00 |
| Comorbidities (n, %) | |||
| T2DM | 13 (46.4%) | 10 (45.5%) | 1.00 |
| Hypertension | 25 (89.2%) | 20 (90.9%) | 1.00 |
| CAD | 1 (3.6%) | 2 (9%) | 0.57 |
| Nutritional state (mean, SD) | |||
| BMI (kg/m2) | 23.2±2.5 | 22.2±3.2 | 0.22 |
| MAC (cm) | 24.3±1.7 | 24.2±4.0 | 0.90 |
| Serum albumin (gm/dL) | 3.6±0.3 | 3.6±0.3 | 1.00 |
| Etiology of ESRD (n, %) | |||
| Diabetic kidney disease | 12 (42.9%) | 6 (27.3%) | 0.37 |
| Chronic glomerulonephritis | 5 (17.9%) | 4 (18.2%) | 1.00 |
| Chronic interstitial disease | 9 (32.1%) | 4 (18.2%) | 0.33 |
| Multiple myeloma-related | 0 | 1 (4.5%) | 0.44 |
| Reflux nephropathy | 0 | 1 (4.5) | 0.44 |
| Unknown | 2 (7.1%) | 6 (27.3%) | 0.11 |
SD: Standard deviation, BMI: Body mass index, MAC: Mid arm circumference, T2DM: Type 2 diabetes mellitus, CAD: Coronary artery disease, ESRD: End-stage renal disease, PDC: Peritoneal dialysis catheter
The cumulative follow-up duration for the coiled-tip cohort was significantly higher than those with straight-tip PDC [Table 2]. The indications of initiation of PD included presentation with advanced symptomatic azotemia or conversion from HD to PD due to either a lack of vascular access or personal preference. Seven patients in either cohort had undergone PD in the past which was discontinued following a mechanical or an infectious complication. Early catheter migration was noted in seven patients with straight-tip PDC; in four patients, the PDC could be salvaged following intervention, while in three, the migration was irreversible necessitating PDC removal [Table 3]. The early PDC migration was significantly less with the use of coiled-tip PDC when compared to straight-tip PDC (3.6% vs. 31.8%; odds ratio (OR): 12.6; 95% confidence interval (CI): 1.41–112.39; P = 0.02) and the numbers needed to treat (NNT) was 4. Late PDC migration was noted in two patients with straight-tip PDC and none in the coiled-tip group (OR: 7.8; 95% CI: 0.35–173.54; P = 0.19). The 1-month and 1-year technique survival in the coiled-tip group was 96.4% and 92.8%, respectively. Of the two catheters lost, one was secondary to early irreversible migration and the second was a consequence of the patient having undergone a live related kidney transplantation 8 months following the initiation of PD. The corresponding 1-month and 1-year technique survival with straight-tip PDC was 86.4% and 77.3%, respectively [Figure 2]. The absolute risk reduction for 1-month and 1-year technique survival with the use of coiled-tip PDC was 10% (95% CI: −5.85 to 25.97) and 6.49% (95% CI: −10.73 to 23.72), respectively. Although the 1-month and 1-year technique survival in the two groups were statistically similar, when the data were reanalyzed after excluding the loss of one coiled-tip PDC due to kidney transplantation, a trend toward favorable 1-year technique survival was noted with the use of coiled-tip PDC (P = 0.07; NNT: 11).

- Kaplan–Meier survival curve depicting the 12-month catheter survival for coiled-tip and straight-tip peritoneal dialysis catheter
| Coiled-tip PDC (n=28) | Straight-tip PDC (n=22) | P | |
|---|---|---|---|
| Indication for PD | |||
| PD first | 11 (39.3%) | 15 (68.2%) | 0.05 |
| Conversion from HD | 17 (60.7%) | 7 (31.8%) | 0.05 |
| Undergone PD in the past (n, %) | 7 (25%) | 7 (31.8%) | 0.75 |
| Duration of HD prior to PD (months) (mean±SD) | 3.2±4.7 | 3.6±7.4 | 0.87 |
| Follow-up duration (months) | |||
| Mean follow-up (±SD) | 20.9±6.7 | 14.6±7.9 | 0.003 |
| Cumulative followup | 585 | 322 |
PD: Peritoneal dialysis, HD: Hemodialysis, PDC: Peritoneal dialysis catheter
| Coiled-tip PDC (n=28) | Straight-tip PDC (n=22) | P | |
|---|---|---|---|
| PDC tip migration | |||
| Early (<8 weeks) | 1 (3.6%) | 7 (31.8%) | 0.01 |
| Late (≥8 weeks) | 0 (0%) | 2 (9.0%) | 0.18 |
| PDC salvaged following intervention | |||
| Early migration | 0 (0%) | 4 (18.2%) | - - |
| Late migration | 0 (0%) | 0 (0%) | - - |
| Technique survival (n, %) | |||
| One-month | 27 (96.4%) | 19 (86.4%) | 0.30 |
| One-year | 26 (92.8%) | 17 (77.3%) | 0.21 |
| Complications (n, %) | |||
| Pericatheter leakage | 3 (10.7%) | 4 (18.2%) | 0.68 |
| Patients with PD peritonitis | 3 (10.7%) | 2 (9.1%) | 1.00 |
| Episodes of PD peritonitis | 7 | 3 | - - |
| Exit site infection | 0 | 0 | - - |
| Tunnel infection | 0 | 0 | - - |
| Cause for technique failure | |||
| Catheter dysfunction with migration | 1 | 5 | 0.07 |
| Catheter dysfunction without migration | 0 | 0 | - - |
| Secondary to peritonitis | 0 | 0 | - - |
| Inadequate dialysis dose | 0 | 0 | - - |
| Genital leak | 0 | 0 | - - |
Therapy-related complications noted in the study included peri-catheter leak and PD peritonitis. External peri-catheter leak necessitating treatment interruption was noted in 10.7% and 18.2% of the coiled-tip and straight-tip groups, respectively. All responded to temporary cessation and re-initiation. Five patients (10 events) developed PD peritonitis: three patients (7 episodes) in the coiled-tip, and two patients (3 episodes) in the straight-tip group. The PD peritonitis rate for the coiled-tip and straight-tip groups was 0.14 and 0.11 events per patient-year, respectively. All responded to administration of appropriate intraperitoneal antibiotics, and none of the PDCs was lost to refractory peritonitis. The sole cause for technique failure in the study was catheter dysfunction with migration; in none, it could be attributed to catheter dysfunction without migration, refractory peritonitis, inadequate dialysis dose, or genital leak.
Discussion
PD is a low-cost, effective therapeutic modality for renal replacement therapy.[6,7] It preserves the RRF and offers a survival advantage in the initial years of dialysis therapy.[8-10] Among the many barriers impeding the successful implementation of a PD program, catheter failure continues to be a major cause for dropout from PD and subsequent conversion to HD. It accounts for 30%–40% of such dropouts, and in a vast majority, this occurs in the first 3 months of PD initiation.[3,4] Thus, there is a need to identify a catheter design that is capable of providing long-term PD access.
Since its introduction in the mid-1960s, the Tenckhoff catheter has been the mainstay of therapy. In an endeavor to improve the outcome, many modifications in the catheter design were introduced. The coiled-tip PDC was designed to ensure better dialysate drainage, reduce migration, and decrease the infusion pain by reducing the jet effect.[11,12] The initial studies using coiled-tip PDC showed better catheter survival when compared to straight-tip PDC.[13] However, the results of the subsequent studies and metanalysis were disappointing.[14,15] Xie et al.[15] randomized 80 patients of coiled versus straight-tip PDC and noted a trend toward increased risk of overall catheter failure in the coiled-tip group. They subsequently pooled their data with existing studies into a metanalysis and noted a significantly higher risk of catheter tip migration with coiled-tip PDC. Similar findings were observed by others.[16] Interestingly, all the studies except one included in this metanalysis utilized surgical techniques; the only study where the percutaneous approach was used showed a superior technique survival with the use of coiled-tip PDC.[13] Thus, it appears that the conclusions derived from surgically placed PDC cannot be extrapolated to those placed percutaneously.
Our study, a retrospective observational study to find the correlation between PDC tip configuration with technique survival showed that the coiled-tip PDC is non-inferior to straight-tip PDC when placed using the guided percutaneous approach. Contrary to the existing studies, we observed fewer early PDC migration and a trend toward improved 1-year technique survival with the use of coiled-tip PDC. Although many center-specific variables, including operator, center characteristics, and catheter placement techniques, are known to influence the outcome,[11] none of these were present in our study, which utilized similar techniques and radio-imaging tools. We attribute our results to the use of the guided percutaneous approach. The use of fluoroscopy by providing real-time visualization ensures appropriate PDC tip placement, and once placed appropriately, the curled-tip PDC by virtue of its bulk fits snugly, reducing the propensity to migrate. Conversely, following an inappropriate initial placement, the same PDC bulk proves disadvantageous, hindering catheter repositioning. Surgical placement being a blind to semi-blind procedure introduces an element of ambiguity with regards to the final PDC placement; this possibly explains the poor technique survival with the use of coiled-tip PDC observed in the earlier studies utilizing the surgical technique. Whether the results reflect operator characteristics, that is, surgeon versus interventional nephrologist, remains debatable. Although the study was not designed to assess the relationship between operator characteristics and the outcome, we feel that the involvement of the treating nephrologist in all the aspects of care (counseling, planning, PDC placement, post-operative care, training, and follow-up) improves the patient satisfaction, compliance, and possibly the therapeutic outcome.
The major cause for technique failure in our study was catheter dysfunction with migration. It was noted in six (12%) patients: five in the straight-tip group and one in the coiled-tip group. Following a migration, it is easier to manipulate and reposition a straight-tip PDC by using conservative and interventional modalities. The guidewire manipulation of coiled-tip PDC is technically challenging, and in our study, the lone migration did not reposition following intervention. None of our patients had technique failure secondary to catheter dysfunction without migration, refractory peritonitis, inadequacy of dialysis dose, or genital leak. Similar findings with noninfectious cause as a major etiology for catheter failure were noted by others.[17] However, many Indian studies have noted peritonitis to be the major cause of technique failure.[18,19]
Although no Indian studies analyzed the relationship between PDC tip design and technique failure, ethnicity and center were thought to be potential confounders. Thus, we correlated our outcome (technique survival) with the existing Indian studies. In their retrospective study involving 46 Indian patients, the authors noted percutaneous insertion of PDC to be a dependable technique, which compared favorably with surgical technique in terms of catheter-related complications.[20] In a retrospective study involving 60 patients (148 patient-years) on PD, the author noted that the overall patient and technique survival at 1, 2, 3, 4, and 5 years was 77%, 53%, 25%, 15%, and 10%, respectively.[18] Peritonitis was noted to be the major cause of technique failure and mortality. In another study involving 148 elderly patients on PD, the technique survival rates, defined as a need to transfer to HS permanently, at 1, 3, and 5 years was noted to be 94.8%, 85.3%, and 71.7%, respectively.[19] They noted peritonitis to be the major cause of technique failure (66.6%), with mechanical complications accounting for 20%. Thus, the 1-year technique survival varied between 77% and 94.8%, and our results were comparable to the existing Indian studies. The major difference was the contribution of peritonitis toward technique failure. While most Indian studies, implicated PD peritonitis as the major cause for technique failure, in our study, only 10% of the patients developed peritonitis and all responded to therapy with no loss of PDC. We attribute this to factors such as structured ongoing training/retraining program, 24 × 7 availability of councilors, early initiation of therapy, strong institutional framework, and younger treatment compliant clientele. Similar to existing studies,[16] we did not find any correlation between the catheter configuration and infection. None of the patients developed exit-site or tunnel infection. This was attributed to the use of preoperative prophylactic antibiotics, minimalistic percutaneous approach, and postoperative care. The higher-than-anticipated incidence of peri-catheter leak in the study was due to chronic urgent-start protocol. The level of education by modulating the reception, assimilation, and execution of training was anticipated to be a potential outcome confounder; however, no correlation was noted in the study. This was likely the result of a simplified uniform hands-on training imparted to all.
Limitation: The study is limited by being a retrospective, non-randomized analysis.
To summarize, the curled-tip PDC when placed using a guided percutaneous approach is associated with fewer early migration and a trend toward favorable long-term technique survival. We feel till more results are available, the most appropriate catheter remains ‘the catheter we are most comfortable with’.
Conclusion
Among the various catheter design, the use of coiled-tip PDC when placed percutaneously reduces early catheter migration and shows a trend toward improved long-term technique survival.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Asystematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int. 2015;88:950-7.
- [Google Scholar]
- Continuous ambulatory peritoneal dialysis:A viable modality of renal replacement therapy in a hilly state of India. Indian J Nephrol. 2007;17:165-9.
- [Google Scholar]
- Chronic peritoneal dialysis catheters:Effect of catheter design, materials and location. Semin Dial. 1990;3:39-46.
- [Google Scholar]
- Time dependent reasons for peritoneal dialysis technique failure and mortality. Perit Dial Int. 2010;30:170-7.
- [Google Scholar]
- Clinical practise guidelines for peritoneal dialysis. Perit Dial Int. 2010;30:424-9.
- [Google Scholar]
- Increasing home-based dialysis therapy to tackle dialysis burden around the world:A position statement on dialysis economics from the 2nd Congress of the International Society of Hemodialysis. Nephrology (Carlton). 2011;16:53-6.
- [Google Scholar]
- Cost analysis of ongoing care of patients with end-stage renal disease:The impact of dialysis modality and dialysis access. Am J Kidney Dis. 2002;40:611-22.
- [Google Scholar]
- Initial survival advantage of peritoneal dialysis relative to hemodialysis. Nephrol Dial Transplant. 2002;17:112-7.
- [Google Scholar]
- Hemodialysis versus peritoneal dialysis:A comparison of adjusted mortality rates. Am J Kidney Dis. 1997;30:334-42.
- [Google Scholar]
- Propensity-matched mortality comparison of incident hemodialysis and peritoneal dialysis patients. J Am Soc Nephrol. 2010;21:499-506.
- [Google Scholar]
- Peritoneal catheters and exit-site practices toward optimum peritoneal access:A review of current developments. Perit Dial Int. 2005;25:132-9.
- [Google Scholar]
- A prospective randomized comparison of the Swan neck, coiled, and straight Tenckhoff catheters in patients on CAPD. Perit Dial Int. 1996;16((Suppl 1)):S333-5.
- [Google Scholar]
- Comparison of straight and curled Tenckhoff peritoneal dialysis catheters implanted by percutaneous technique:A prospective randomized study. Perit Dial Int. 1995;15:18-21.
- [Google Scholar]
- Comparing the incidence of catheter-related complications with straight and coiled Tenckhoff catheters in peritoneal dialysis patients—a single-center prospective randomized trial. Perit Dial Int. 2015;35:443-9.
- [Google Scholar]
- Coiled versus straight peritoneal dialysis catheters:A Randomized controlled trial and meta-analysis. Am J Kidney Dis. 2011;58:946-55.
- [Google Scholar]
- A systematic review and meta-analysis of the influence of peritoneal dialysis catheter type on complication rate and catheter survival. Kidney Int. 2014;85:920-32.
- [Google Scholar]
- Risk factors associated with peritoneal dialysis catheter survival:A 9-year single-center study in 315 patients. J Vasc Access. 2010;11:316-22.
- [Google Scholar]
- Long-term clinical outcomes of peritoneal dialysis patients:9-year experience of a single center from north India. Perit Dial Int. 2014;34:426-33.
- [Google Scholar]
- Clinical characteristics, patient and technique survival in elderly patients on peritoneal dialysis. Indian J Nephrol. 2019;29:334-9.
- [Google Scholar]
- Percutaneous CAPD catheter insertion by a nephrologist versus surgical placement:A comparative study. Indian J Nephrol. 2008;18:5-8.
- [Google Scholar]







